Urinary incontinence
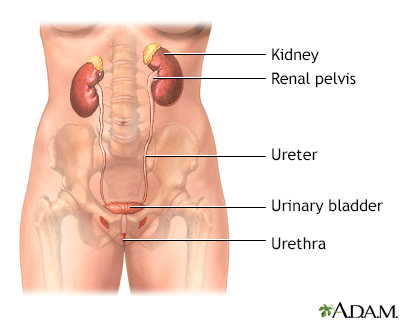
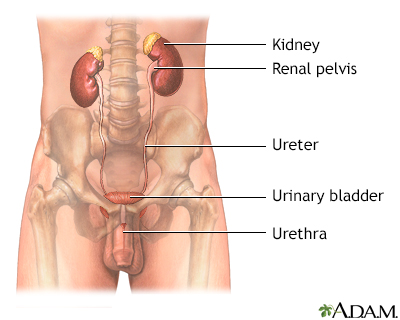
Urinary (or bladder) incontinence occurs when you are not able to keep urine from leaking out of your urethra. The urethra is the tube that carries urine out of your body from your bladder. You may leak urine from time to time. Or, you may not be able to hold any urine.
Urinary incontinence - Animation
When you enter a store or restaurant, are you often looking to find the establishments bathroom? If you're having trouble holding in your urine, or if you often leak urine, you probably have what's called urinary incontinence. Normally, the bladder begins to fill with urine from the kidneys. The bladder stretches to allow more and more urine. You should feel the first urge to urinate when there is about 200 mL, just under 1 cup of urine stored in your bladder. A healthy nervous system will respond to this stretching sensation by letting you know that you have to urinate. But, at the same time, the bladder should keep filling. But the system doesn't work correctly in people with urinary incontinence. Some people with urinary incontinence leak urine during activities like coughing, sneezing, laughing, or exercise. This is called stress incontinence. When you have a sudden, strong need to urinate, but can't make it to the bathroom before you do urinate, it's called urge incontinence. Other people have what's called overflow incontinence, when the bladder cannot empty and they dribble. Urinary incontinence can have many causes, and it's most common in older adults. Women are more likely than men to have it. For some people the bladder muscle is overactive. For others, the muscles holding the urine in are weak. And for others, the problem is sensing when the bladder is full. They might have brain or nerve problems, dementia or other health problems that make it hard to feel and respond to the urge to urinate, or problems with the urinary system itself. To treat urinary incontinence, your doctor can help you form a treatment plan. Most likely, exercises to strengthen the muscles of your pelvic floor will be part of that plan. Bladder training exercises can also be effective. And depending on the cause of incontinence, oral medications, or topical estrogen may be helpful. If you have overflow incontinence and cannot empty your bladder completely, you may need to use a catheter. Your doctor can recommend the best catheter for you. For urine leaks, you might wear absorbent pads or undergarments. Whatever else you try, lifestyle changes may help. Aim for an ideal weight. Losing excess weight and increasing exercise both often improve incontinence, especially in women. Also, some specific beverages and foods might increase leaking in some people. For instance, you might try eliminating alcohol, caffeine, carbonated beverages, even decaf coffee. Drink plenty of water, but do NOT drink anything 2 to 4 hours before going to bed. Be sure to empty your bladder before going to bed to help prevent urine leakage at night. Throughout the day, urinate at set times, even if you do not feel the urge. Schedule yourself every 3 to 4 hours. Urinary incontinence is very common, but many people never talk to their doctor about it. Don't let that be you. See your doctor and bring it up at your next doctor's visit.
The three main types of urinary incontinence are:
- Stress incontinence -- occurs during activities like coughing, sneezing, laughing, or exercise.
Stress incontinence
Stress urinary incontinence occurs when your bladder leaks urine during physical activity or exertion. It may happen when you cough, sneeze, lift so...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urge incontinence -- occurs as a result of a strong, sudden need to urinate immediately. Then the bladder squeezes and you lose urine. You don't have enough time after you feel the urge to urinate to get to the bathroom before you begin urinating.
Urge incontinence
Urge incontinence occurs when you have a strong, sudden need to urinate that is difficult to delay. The bladder then squeezes, or spasms, and you ma...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Overflow incontinence -- occurs when the bladder does not empty and the volume of urine exceeds its capacity. This leads to dribbling.
Mixed incontinence occurs when you have more than one type of incontinence, usually both stress and urge urinary incontinence.
Bowel incontinence is when you are unable to control the passage of stool. It is not covered in this article.
Bowel incontinence
Bowel incontinence is the loss of bowel control, causing you to unexpectedly pass stool. This can range from sometimes leaking a small amount of sto...

Causes
Causes of urinary incontinence include:
- Blockage in the urinary system
- Brain or nerve problems
- Dementia or other mental health problems that make it hard to feel and respond to the urge to urinate
- Problems with the urinary system
- Nerve and muscle problems
- Weakness of the pelvic or urethral muscles
- Enlarged prostate
- Diabetes
- Use of certain medicines
Incontinence may be sudden and go away after a short period of time. Or, it may continue long-term. Causes of sudden or temporary incontinence include:
- Bedrest -- such as when you are recovering from surgery
- Certain medicines (such as diuretics, antidepressants, tranquilizers, some cough and cold remedies, and antihistamines)
- Mental confusion
- Pregnancy
- Prostate infection or inflammation
- Stool impaction from severe constipation, which causes pressure on the bladder
Impaction
A fecal impaction is a large lump of dry, hard stool that stays stuck in the rectum. It is most often seen in people who are constipated for a long ...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Urinary tract infection or inflammation
Urinary tract infection
A urinary tract infection, or UTI, is an infection of the urinary tract. The infection can occur at different points in the urinary tract, including...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Weight gain
Causes that may be more long-term include:
- Alzheimer disease.
Alzheimer disease
Dementia is a loss of brain function that occurs with certain diseases. Alzheimer disease (AD) is the most common form of dementia. It affects memo...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Bladder cancer.
- Bladder spasms.
- Large prostate in men.
- Nervous system conditions, such as multiple sclerosis or stroke.
- Nerve or muscle damage after radiation treatment to the pelvis.
- Pelvic prolapse in women which is falling or sliding of the bladder, urethra, or rectum into the vagina. This may be caused by pregnancy and delivery.
- Problems with the urinary tract.
- Spinal cord injuries.
- Weakness of the urinary sphincter, the circle-shaped muscles that open and close the bladder. This can be caused by prostate surgery in men, or surgery to the vagina in women.
Home Care
If you have symptoms of incontinence, see your health care provider for evaluation, tests, and a treatment plan. Which treatment you get depends on what caused your incontinence and what type you have.
There are several treatment approaches for urinary incontinence:
Lifestyle changes. These changes may help improve incontinence. You may need to make these changes along with other treatments.
- Keep your bowel movements regular to avoid constipation. Try increasing the fiber in your diet.
- Quit smoking to reduce coughing and bladder irritation. Smoking also increases your risk for bladder cancer.
- Avoid alcohol and caffeinated drinks such as coffee, which can stimulate your bladder.
- Lose weight if you need to.
- Avoid foods and drinks that may irritate your bladder. These include spicy foods, carbonated drinks, and citrus fruits and juices.
- If you have diabetes, keep your blood sugar under good control.
For urine leaks, wear absorbent pads or undergarments. There are many well-designed products that no one else will notice.
Well-designed products
There are many products to help you manage urinary incontinence. You can decide which product to choose based on:How much urine you loseComfortCostD...

Bladder training and pelvic floor exercises. Bladder retraining helps you gain better control over your bladder. Kegel exercises can help strengthen the muscles of your pelvic floor. Your provider can show you how to do them. Many women do not do these exercises correctly, even if they believe they are doing them correctly. Often, people benefit from formal bladder strengthening and retraining with a pelvic floor specialist.
Medicines. Depending on the type of incontinence you have, your provider may prescribe one or more medicines. These medicines help prevent bladder muscle spasms, relax the bladder, and improve bladder function. Your provider can help you learn how to take these medicines and manage their side effects.
Surgery. If other treatments do not work, or you have severe incontinence, your provider may recommend surgery. The type of surgery you have will depend on:
- The type of incontinence you have (such as urge, stress, or overflow)
Urge
Urge incontinence occurs when you have a strong, sudden need to urinate that is difficult to delay. The bladder then squeezes, or spasms, and you ma...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleStress
Stress urinary incontinence occurs when your bladder leaks urine during physical activity or exertion. It may happen when you cough, sneeze, lift so...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - The severity of your symptoms
- The cause (such as pelvic prolapse, enlarged prostate, enlarged uterus, or other causes)
Enlarged prostate
The prostate is a gland that produces some of the fluid that carries sperm during ejaculation. The prostate gland surrounds the urethra, the tube th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
If you have overflow incontinence or you cannot fully empty your bladder, you may need to use a urinary catheter. You may use a catheter that stays in your bladder long-term, or one that you are taught to put in and take out yourself.
Catheter
You have an indwelling catheter (tube) in your bladder. "Indwelling" means inside your body. This catheter drains urine from your bladder into a ba...
Read Article Now Book Mark ArticleBladder nerve stimulation. Urge incontinence and urinary frequency can sometimes be treated by electrical nerve stimulation. Pulses of electricity are used to reprogram bladder reflexes. In one technique, the provider inserts a stimulator through the skin near a nerve in the leg. This is done weekly in the provider's office. Another method uses battery-operated implanted device similar to a pacemaker that is placed under the skin in the lower back.
Botox injections. Urge incontinence can sometimes be treated with an injection of onabotulinum A toxin (also known as Botox). The injection relaxes the bladder muscle and increases the storage capacity of the bladder. The injection is delivered through a thin tube with a camera on the end (cystoscope). In most cases, the procedure can be done in the provider's office.
When to Contact a Medical Professional
Talk to your provider about incontinence. Some providers who treat incontinence are gynecologists and urologists that specialize in this problem. They can find the cause and recommend treatments.
Call your local emergency number (such as 911) or go to an emergency room if you suddenly lose control over urine and you have:
- Difficulty talking, walking, or speaking
- Sudden weakness, numbness, or tingling in an arm or leg
- Loss of vision
- Loss of consciousness or confusion
- Loss of bowel control
Contact your provider if you have:
- Cloudy or bloody urine
- Dribbling
- Frequent or urgent need to urinate
- Pain or burning when you urinate
- Trouble starting your urine flow
- Fever
Reviewed By
Kelly L. Stratton, MD, FACS, Associate Professor, Department of Urology, University of Oklahoma Health Sciences Center, Oklahoma City, OK. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Heesakkers JPFA, Blok B. Electrical stimulation and neuromodulation in storage and emptying failure. In: Partin AW, Dmochowski RR, Kavoussi LR , Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 122.
Lentz GM, Miller JL. Lower urinary tract function and disorders: physiology of micturition, voiding dysfunction, urinary incontinence, urinary tract infections, and painful bladder syndrome. In: Gershenson DM, Lentz GM, Valea FA, Lobo RA, eds. Comprehensive Gynecology. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 21.
Newman DK, Burgio KL. Conservative management of urinary incontinence: behavioral and pelvic floor therapy, urethral and pelvic devices. In: Partin AW, Dmochowski RR, Kavoussi LR, Peters CA, eds. Campbell-Walsh-Wein Urology. 12th ed. Philadelphia, PA: Elsevier; 2021:chap 121.
Resnick NM, DuBeau CE. Urinary incontinence. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 115.
Reynolds WS, Dmochowski R, Karram MM, Mahdy A. Surgical management of refractory overactive bladder and detrusor compliance abnormalities. In: Baggish MS, Karram MM, eds. Atlas of Pelvic Anatomy and Gynecologic Surgery. 5th ed. Philadelphia, PA: Elsevier; 2021:chap 90.


 All rights reserved.
All rights reserved.