Cholesterol - drug treatment
Your body needs cholesterol to work properly. But extra cholesterol in your blood causes deposits to build up on the inside walls of your blood vessels. This buildup is called plaque. It narrows your arteries and can reduce or stop blood flow. This can lead to heart attack, stroke, and narrowing of the arteries elsewhere in your body.
Extra cholesterol in your blood
Cholesterol is a fat (also called a lipid) that your body needs to work properly. Too much bad cholesterol in your blood can increase your chance of...
Statins are thought to be the best drugs to use for people who need medicines to lower their cholesterol.
Alternative names
Hyperlipidemia - drug treatment; Hardening of the arteries - statin
Statins for Cholesterol
Statins reduce your risk of heart disease, stroke, and other related problems. They do this by lowering your LDL (bad) cholesterol.
Most of the time you will need to take this medicine for the rest of your life. In some cases, changing your lifestyle and losing extra weight may allow you to stop taking this medicine.
Changing your lifestyle
Your body needs cholesterol to work well. But cholesterol levels that are too high can harm you. In the US, blood cholesterol is most often measured...
Who Should Take Statins to Lower Cholesterol?
Having low LDL and total cholesterol reduces your risk of heart disease. But not everyone needs to take statins to lower cholesterol.
Your health care provider will recommend your treatment based on:
- Your total, HDL (good), and LDL (bad) cholesterol levels
- Your age
- Your history of diabetes, high blood pressure, or heart disease
- Other health problems that may be caused by high cholesterol
- Whether or not you smoke
- Your risk of heart disease
- Your ethnicity
You should take statins if you are 75 or younger, and you have a history of:
- Heart problems due to narrowed arteries in the heart
- Stroke or TIA (mini stroke)
- Aortic aneurysm (a bulge in the main artery in your body)
- Narrowing of the arteries to your legs
If you are older than 75, your provider may prescribe a lower dose of a statin. This may help lessen possible side effects.
You should take statins if your LDL cholesterol is 190 mg/dL (4.92 mmol/L) or higher. You should also take statins if your LDL cholesterol is 70 to 189 mg/dL (1.81 to 4.90 mmol/L) and:
- You have diabetes and are between ages 40 and 75
- You have diabetes and a high risk of heart disease
- You have a high risk of heart disease
You and your provider may want to consider statins if your LDL cholesterol is 70 to 189 mg/dL (1.81 to 4.90 mmol/L) and:
- You have diabetes and a medium risk for heart disease
- You have a medium risk for heart disease
If you have a high risk for heart disease and your LDL cholesterol stays high even with statin treatment, your provider may consider these drugs in addition to statins:
- Ezetimibe
- PCSK9 inhibitors, such as alirocumab and evolocumab (Repatha)
How low Should Your LDL Cholesterol be?
Providers used to set a target level for your LDL cholesterol. But now the focus is reducing your risk for problems caused by narrowing of your arteries. Your provider may monitor your cholesterol levels. But frequent testing is rarely needed.
You and your provider will decide what dose of a statin you should take. If you have risk factors, you may need to take higher doses. or add other types of drugs. Factors that your provider will consider when choosing your treatment include:
- Your total, HDL, and LDL cholesterol levels before treatment
- Whether you have coronary artery disease (history of angina or heart attack), a history of stroke, or narrowed arteries in your legs
- Whether you have diabetes
- Whether you smoke or have high blood pressure
Higher doses may lead to side effects over time. So your provider will also consider your age and risk factors for side effects.
References
American Heart Association website. Cholesterol medications. www.heart.org/en/health-topics/cholesterol/prevention-and-treatment-of-high-cholesterol-hyperlipidemia/cholesterol-medications. Updated February 20, 2024. Accessed March 5, 2024.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the primary prevention of cardiovascular disease: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019;140(11):e596-e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S179-S218. PMID: 38078592 pubmed.ncbi.nlm.nih.gov/38078592/.
Genest J, Mora S, Libby P. Lipoprotein disorders and cardiovascular disease. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 27.
Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2019;73(24): 3234-3237. PMID: 30423391 pubmed.ncbi.nlm.nih.gov/30423391/.
Joseph JJ, Deedwania P, Acharya T, et al. American Heart Association Diabetes Committee of the council on lifestyle and cardiometabolic health; council on arteriosclerosis, thrombosis and vascular biology; council on clinical cardiology; and council on hypertension. comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement from the American Heart Association. Circulation. 2022;145(9):e722-e759. PMID: 35000404 pubmed.ncbi.nlm.nih.gov/35000404/.
US Preventive Services Task Force; Mangione CM, Barry MJ, et al. Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force Recommendation Statement. JAMA. 2022;328(8):746-753. PMID: 35997723 pubmed.ncbi.nlm.nih.gov/35997723/.
-
Types of hyperlipidemia
Animation
-
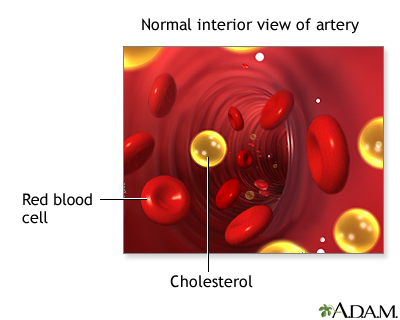
Cholesterol - illustration
Cholesterol is a soft, waxy substance that is present in all parts of the body including the nervous system, skin, muscle, liver, intestines, and heart. It is made by the body and obtained from animal products in the diet. Cholesterol is manufactured in the liver and is needed for normal body functions including the production of hormones, bile acid, and Vitamin D. Excessive cholesterol in the blood contributes to atherosclerosis and subsequent heart disease. The risk of developing heart disease or atherosclerosis increases as the level of blood cholesterol increases.
Cholesterol
illustration
-
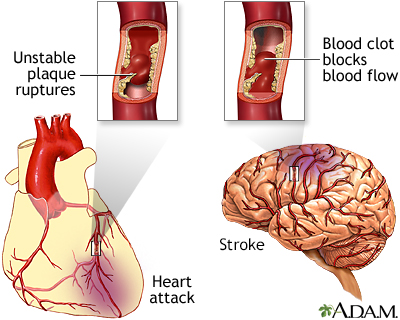
Plaque buildup in arteries - illustration
A heart attack or stroke may occur when an area of plaque (atherosclerosis) ruptures and a clot forms over the location, blocking the flow of blood to the organ's tissues.
Plaque buildup in arteries
illustration
-
Cholesterol - illustration
Cholesterol is a soft, waxy substance that is present in all parts of the body including the nervous system, skin, muscle, liver, intestines, and heart. It is made by the body and obtained from animal products in the diet. Cholesterol is manufactured in the liver and is needed for normal body functions including the production of hormones, bile acid, and Vitamin D. Excessive cholesterol in the blood contributes to atherosclerosis and subsequent heart disease. The risk of developing heart disease or atherosclerosis increases as the level of blood cholesterol increases.
Cholesterol
illustration
-
Plaque buildup in arteries - illustration
A heart attack or stroke may occur when an area of plaque (atherosclerosis) ruptures and a clot forms over the location, blocking the flow of blood to the organ's tissues.
Plaque buildup in arteries
illustration
-
Hypercholesterolemia
(Alt. Medicine)
-
Cholesterol - InDepth
(In-Depth)
-
Atherosclerosis
(Alt. Medicine)
-
Myocardial infarction
(Alt. Medicine)
-
Psoriasis-In-Depth
(In-Depth)
Review Date: 2/27/2024
Reviewed By: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.