Heart attack and acute coronary syndrome - InDepth
Heart attack - ACS - InDepth; Myocardial infarction - ACS - InDepth; MI - ACS - InDepth; Acute MI - ACS - InDepth; ST elevation myocardial infarction - ACS - InDepth; Non ST-elevation myocardial infarction - ACS - InDepth; Unstable angina - ACS - InDepth; Accelerating angina - ACS - InDepth; Angina - unstable-ACS - InDepth; Progressive angina - InDepth; Acute coronary syndrome - InDepth; Myocardial infarction - InDepth; MI - InDepth; Acute MI - InDepth; ST-elevation myocardial infarction - InDepth; Non-ST-elevation myocardial infarction - InDepth; NSTEMI - InDepth; CAD - heart attack - InDepth; Coronary artery disease - heart attack - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of heart attack.
Highlights
Heart Attack Symptoms
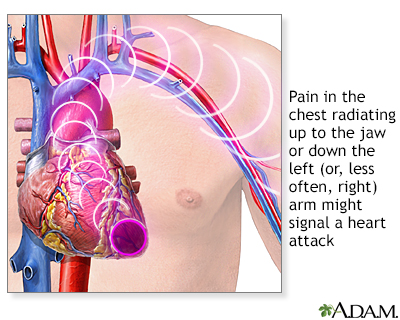
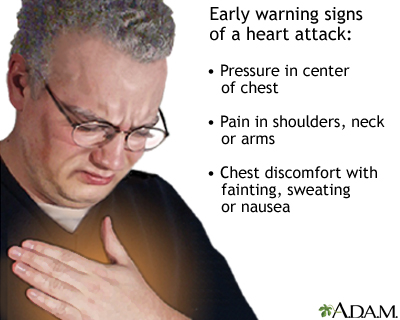
Common signs and symptoms of heart attack include:
- Chest pain or discomfort (angina), which can feel like pressure, squeezing, fullness, or pain in the center of the chest. With a heart attack, the pain usually lasts for more than a few minutes. But it may increase and decrease in intensity.
- Discomfort in the upper body including the arms, neck, back, jaw, or stomach.
- Shortness of breath, which can occur with or without chest pain.
- Nausea and vomiting.
- Breaking out in a cold sweat.
- Lightheadedness or fainting.
- Women (and some men) may have atypical symptoms such as abdominal distress, nausea, palpitations, and fatigue without chest pain. Older adults and people with diabetes also often have atypical symptoms.
Immediate Treatment of a Heart Attack Patient
If you think you are having a heart attack, call 911 or the local emergency number right away and wait for an ambulance. DO NOT attempt to drive yourself to the hospital. After you call 911 or the local emergency number, chew an adult-size (325 mg) non-coated aspirin. Be sure to tell the paramedics so an additional aspirin dose is not given.
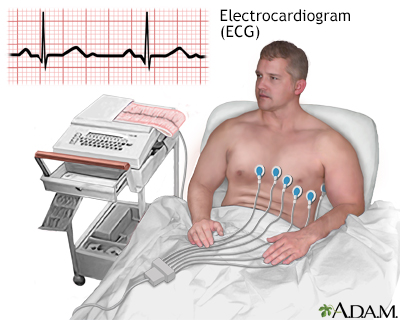
For a particular type of heart attack called ST-elevation myocardial infarction or STEMI, which is diagnosed by electrocardiography (ECG or EKG), guidelines recommend:
- Angioplasty (almost always with stenting), also called percutaneous coronary intervention (PCI), is a procedure that should be performed within 90 minutes of arriving at the hospital. People suffering a heart attack should be transported by emergency services to hospitals equipped to perform PCI, if possible.
- Fibrinolytic ("clot-busting") therapy should be given if a center that performs PCI is not available or if anticipated transfer time would exceed a certain window of time and there are no contraindications for fibrinolysis.
Secondary Prevention of Heart Attack
Secondary prevention measures are essential to help prevent another heart attack. DO NOT leave the hospital without discussing these secondary prevention steps with your doctor:
- High blood pressure and cholesterol control. (Nearly all people who have had a heart attack should be discharged from the hospital with a prescription for a statin drug, an ACE inhibitor, and a beta blocker).
- Low-dose (81 mg) aspirin, which most people will need to take on an ongoing basis. People who cannot tolerate aspirin may take another type of antiplatelet drug such as clopidogrel (Plavix, generic). People who have had angioplasty/PCI along with drug-eluting stent placement will usually need an additional antiplatelet medication along with aspirin for at least a year following the procedure.
- Cardiac rehabilitation, which includes a regular exercise program.
- Heart-healthy diet and weight management.
- Smoking cessation and avoidance of secondhand tobacco smoke.
- An annual influenza (flu) vaccine.
Aspirin for Heart Attack Prevention
The American Heart Association recommends daily low-dose aspirin for:
- Primary prevention of heart attack and stroke in people who are at risk for heart disease (when a doctor says to take aspirin).
- Secondary prevention of heart attack and stroke in people who have already had a heart attack or stroke.
- In 2014, the FDA advised that daily aspirin use for primary prevention (people without disease) of cardiovascular disease should be an individual clinical judgment between providers and people weighing the risks of bleeding against the benefits of prevention. This is because daily aspirin use can increase the risk for bleeding. For most people who have existing heart problems, the benefits of aspirin outweigh the risks. Always check with your doctor before starting or stopping daily aspirin.
Introduction
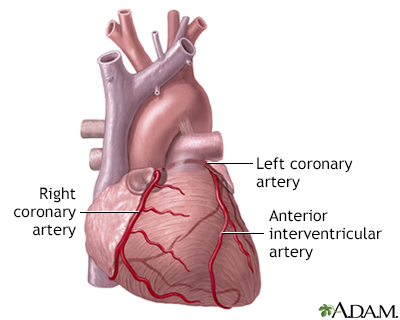
The heart is the body's hardest working organ. Throughout life, it continuously pumps blood enriched with oxygen and vital nutrients through a network of arteries to all tissues of the body. To perform this strenuous task, the heart muscle itself needs a plentiful supply of oxygen-rich blood, provided through a network of coronary arteries. These arteries carry oxygen-rich blood to the heart's muscular walls (the myocardium).
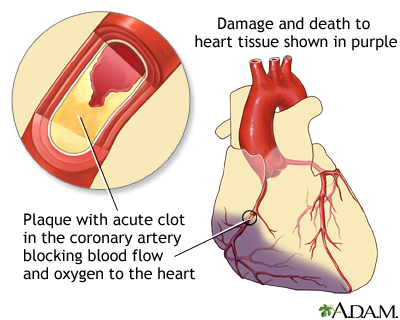
A heart attack (myocardial infarction) occurs when blood flow to the heart muscle is blocked, and tissue death occurs from loss of oxygen, severely damaging a portion of the heart.
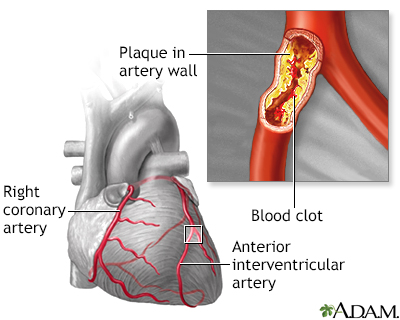
Atherosclerosis is the hardening and narrowing of the arteries caused by the build-up of plaque inside the walls of the arteries. (Plaque is the sticky substance made up of fat, cholesterol, calcium, and other substances found in the blood.) Cardiovascular diseases caused by atherosclerosis include coronary artery disease, heart attack, peripheral artery disease, and stroke.
Coronary Artery Disease
An in-depth report on the causes, diagnosis, treatment, and prevention of coronary artery disease (CAD).

| Read Article Now | Book Mark Article |
Coronary artery disease causes nearly all heart attacks. Coronary artery disease is the result of a complex process called atherosclerosis. This is the narrowing of arteries by fat deposits called plaque that causes blockage of arteries (ischemia) and prevents oxygen-rich blood from reaching the heart.
Heart Attack
Heart attack (myocardial infarction) is among the most serious outcome of atherosclerosis. A heart attack can result in several ways from atherosclerosis:
- Type 1 heart attack occurs when the plaque develops fissures or tears. Blood platelets stick to the tears to seal off the plaque, and a blood clot (thrombus) forms. A heart attack can then occur if the blood clot severely or completely blocks blood flow to the heart.
- Type 2 heart attack, which is less common, develops from a problem with oxygen supply and demand. A heart attack can occur if the heart's oxygen demand increases to exceed the artery's ability to deliver oxygen-rich blood even without a sudden new narrowing or blockage.
Angina
Angina, the primary symptom of coronary artery disease, is typically experienced as chest pain. There are two kinds of angina:
- Stable Angina. This is predictable chest pain that occurs in a certain situation such as with walking briskly or upstairs, and is relieved with rest. It often can be managed with lifestyle changes and medications to prevent heart attacks and disease progression, and to control the chest pain. Drugs include low-dose aspirin, lipid-lowering agents, beta blockers, calcium channel blockers, and nitrates.
- Unstable Angina. This situation is much more serious than stable angina, and is often an intermediate stage between stable angina and a heart attack. In this condition, people who have previously had stable angina have worsening symptoms. For example, their pain is more intense or it takes less activity to trigger symptoms or it may be totally new. They may even have symptoms while at rest. Unstable angina is one type of acute coronary syndrome.
Acute Coronary Syndromes (ACS)
Acute coronary syndromes (ACS) are a group of severe and sudden heart conditions that need urgent/emergent and aggressive treatment. ACS includes:
- Unstable Angina. Unstable angina is diagnosed when there is new or worsened chest pain consistent with angina sometimes with ECG changes, but blood tests DO NOT show markers for heart attack. Unstable angina is often considered a precursor to a heart attack.
- NSTEMI (Non ST-segment Elevation Myocardial Infarction). This condition is diagnosed when similar symptoms and ECG changes are seen as with unstable angina, but blood tests are positive for heart muscle damage.
- STEMI (ST-segment Elevation Myocardial Infarction). This condition is diagnosed when angina is described and specific ECG changes and blood tests confirm a heart attack. This type of heart attack involves the full thickness of a portion of the heart muscle.
People diagnosed with an ACS are at risk for complications. Doctors use a person's medical history, various tests, and the presence of certain factors to help predict which ACS patients are most at risk for developing a more serious condition. The severity of chest pain itself does not necessarily indicate the actual amount of damage to the heart.
Risk Factors
The risk factors for heart attack are the same as those for coronary artery disease (heart disease). They include:
Age
The risks for coronary artery disease increase with age. About 85% of people who die from heart disease are over the age of 65. For men, the average age of a first heart attack is 66 years.
Gender
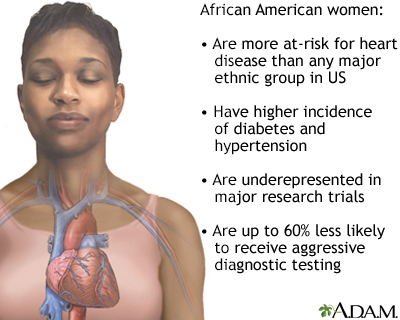
Men have a greater risk for coronary artery disease overall, and are more likely to have heart attacks earlier in life than women. However, women's risk for heart disease increases after menopause (typically 10 years later than men) so that after the age of 75 years the majority of heart attack patients are women, and cardiovascular diseases are the most common cause of death and disability in women in the US.
Genetic Factors and Family History
Certain genetic factors increase the likelihood of developing important risk factors, such as diabetes, elevated cholesterol, and high blood pressure.
Race and Ethnicity
African Americans have the highest risk of heart disease in part due to their high rates of severe high blood pressure as well as diabetes and obesity.
Medical Conditions
Obesity and Metabolic Syndrome
Excess body fat, particularly around the waist, can increase the risk for heart disease. Obesity also increases the risk for other conditions (such as high blood pressure and diabetes) that are associated with heart disease. Obesity is particularly hazardous when it is part of the metabolic syndrome, a pre-diabetic condition that is significantly associated with heart disease. This syndrome is diagnosed when three of the following are present:
Diabetes
An in-depth report on the causes, diagnosis, treatment, and prevention of type 2 diabetes.

| Read Article Now | Book Mark Article |
- Abdominal obesity
- Low HDL cholesterol
- High triglyceride levels
- High blood pressure
- Insulin resistance (diabetes or pre-diabetes)
There are many non-medication ways to control your weight and improve aspects of the metabolic syndrome, such as diet and exercise.
Control your weight
An in-depth report on the causes, diagnosis, treatment, and prevention of lupus.

| Read Article Now | Book Mark Article |
Unhealthy Cholesterol Levels
Low-density lipoprotein (LDL) cholesterol is the "bad" cholesterol responsible for many heart problems. Triglycerides are another type of lipid (fat molecule) that can be bad for the heart. High-density lipoprotein (HDL) cholesterol is the "good" cholesterol that helps protect against heart disease. Doctors test for a lipid profile that includes measurements for total cholesterol, LDL, HDL, and triglycerides. The ratio of these lipids can affect heart disease risk. New guidelines for cholesterol treatment focus on reducing a person's overall risk for or from cardiovascular disease, rather than aiming for a target cholesterol number.
Cholesterol
An in-depth report on the diagnosis, treatment, and prevention of unhealthy cholesterol levels.

| Read Article Now | Book Mark Article |
High Blood Pressure
High blood pressure (hypertension) is associated with coronary artery disease and heart attack. For an adult, a normal blood pressure reading is below 120/80 mm Hg. Blood pressure readings of 120 to 129 systolic (but diastolic <80 mm Hg) are referred to as "elevated blood pressure" and "hypertension" is diagnosed for established blood pressure readings greater than or equal to 130 mm Hg (systolic) or greater than or equal to 80 mm Hg (diastolic).
High blood pressure
An in-depth report on the causes, diagnosis, treatment, and prevention of high blood pressure.

| Read Article Now | Book Mark Article |
Diabetes
Diabetes, particularly for people whose blood sugar levels are not well controlled, significantly increases the risk of developing heart disease. In fact, heart disease and stroke are the leading causes of death in people with diabetes. People with diabetes, both type 1 (so-called "juvenile") and type 2 (so-called "adult onset"), are also at risk for high blood pressure and unhealthy cholesterol levels, blood clotting problems, kidney disease, and impaired nerve function, all of which can damage the heart.
Type 1
An in-depth report on the causes, diagnosis, and treatment of type 1 diabetes.

| Read Article Now | Book Mark Article |
Type 2
An in-depth report on the causes, diagnosis, treatment, and prevention of type 2 diabetes.

| Read Article Now | Book Mark Article |
Lifestyle Factors
Physical Inactivity
Exercise has a number of effects that benefit the heart and circulation, including improving cholesterol levels and blood pressure and maintaining weight control. People who are sedentary are almost twice as likely to suffer heart attacks as are people who exercise regularly.
Smoking
Smoking is the most important lifestyle risk factor for heart disease. Smoking can cause elevated blood pressure, worsen lipids, and make platelets very sticky, raising the risk of clots. Although heavy cigarette smokers are at greatest risk, people who smoke as few as 3 cigarettes a day are at higher risk for blood vessel abnormalities that endanger the heart. Regular exposure to passive smoke also increases the risk of heart disease in non-smokers. For people who have had a heart attack, continuing to smoke increases the risk of death from another heart attack.
Smoking
An in-depth report on the health risks of smoking and how to quit.

| Read Article Now | Book Mark Article |
Alcohol
Moderate alcohol consumption (one or two glasses a day) can help boost HDL (good) cholesterol levels. Alcohol may also prevent blood clots and inflammation. By contrast, heavy drinking harms the heart. In fact, heart disease is the leading cause of death in alcoholics.
Diet
Diet can play an important role in protecting the heart. Particularly beneficial is reducing the intake of trans fats, saturated fats, and cholesterol and restricting salt intake that contributes to high blood pressure.
Diet can play an important role in protecting t...
An in-depth report on how to build the best diet for your heart's health.

| Read Article Now | Book Mark Article |
NSAIDs and COX-2 Inhibitors
All nonsteroidal anti-inflammatory drugs (NSAIDs) -- with the exception of aspirin -- carry heart risks. NSAIDs and COX-2 inhibitors may increase the risk for death in people who have experienced a heart attack. The risk is greatest at higher dosages. But some research suggests that even low doses of NSAIDs taken for short periods of time are not safe after a heart attack.
NSAIDs include nonprescription drugs like ibuprofen (Advil, Motrin, generic) and prescription drugs like diclofenac (Cataflam, Voltaren, generic). Celecoxib (Celebrex) is currently the only COX-2 inhibitor that is available in the US. It has been linked to cardiovascular risks, such as heart attack and stroke. People who have had heart attacks should talk to their doctors before taking any of these drugs.
The American Heart Association recommends that people who have, or who are at risk for, heart disease first try non-drug methods of pain relief (such as physical therapy, exercise, weight loss to reduce stress on joints, and heat or cold therapy). If these methods don't work, people should take the lowest effective and safe dose of acetaminophen (Tylenol, generic) or aspirin before using an NSAID. The COX-2 inhibitor celecoxib (Celebrex) should be a last resort.
Prognosis
Heart attacks may be rapidly fatal, evolve into a chronic disabling condition, or lead to full recovery. The long-term prognosis for both length and quality of life after a heart attack depends on its severity, the amount of damage sustained by the heart muscle, the preventive measures taken afterward, and the prior health status of the person.
People who have had a heart attack have a higher risk of a second heart attack. Although no tests can absolutely predict whether another heart attack will occur, people can reduce their risk of having another heart attack by healthy lifestyle changes and adherence to medical treatments.
Heart attack also increases the risk for other heart problems, including heart failure, abnormal heart rhythms, heart valve damage, and stroke.
Higher Risk Individuals
A heart attack is always more serious in certain people, including:
- Older people
- People with a history of heart disease or multiple risk factors for heart disease
- People with heart failure
- People with diabetes
- People with multiple other medical problems
Women are more likely to die from a heart attack than men. The gender difference is greatest for younger people.
Factors Occurring at the Time of a Heart Attack That Increase Severity
The presence of other conditions during a heart attack can contribute to a poorer outlook:
- Arrhythmias are abnormal heart rhythms. A particularly dangerous arrhythmia called ventricular fibrillation is a major cause of early death from heart attack. Arrhythmias are more likely to occur within the first several hours of a heart attack, and they are associated with a high mortality rate. However, people who are successfully treated have the same long-term prognosis as those who DO NOT have such arrhythmias.
- Heart block, also called atrioventricular (AV) block, is a type of arrhythmia in which the electric conduction of nerve impulses to muscles in the heart is slowed or interrupted. Although heart block is dangerous, it can be treated effectively with a pacemaker, and it rarely causes any long-term complications in patients who survive it.
- Cardiogenic shock is a very dangerous condition that is associated with very low blood pressure, reduced urine levels, and other abnormalities throughout the body. Shock occurs in about 7% of heart attacks and results from so much of the heart being damaged that it cannot pump effectively or another complication such as damage to a heart valve.
- Heart failure is a condition in which the damaged heart muscle is unable to pump all the blood that the tissues need. People experience fatigue, shortness of breath, and fluid buildup. When heart failure is severe it can lead to shock (very low blood pressure).
Symptoms
Heart Attack Symptoms
Heart attack symptoms can vary. They may come on suddenly and severely or may progress slowly, beginning with mild pain. Although chest pain is the classic symptom associated with heart attack, a third of people DO NOT experience this symptom.
Symptoms can vary between men and women. Women, older people, and people with diabetes are less likely to have chest pain. But they are more likely to experience shortness of breath, nausea or vomiting, or jaw and back pain.
Common signs and symptom of heart attack include:
- Chest pain. Chest pain or discomfort (angina) is the main sign of a heart attack. It can feel like pressure, squeezing, fullness, or pain in the center of the chest. Often the pain radiates to the neck, jaw, shoulder, or down the left arm. People with coronary artery disease who have stable angina often experience chest pain that lasts for a few minutes and then goes away. With heart attack, the pain is intense and usually lasts for more than a few minutes (typically 30 to 60 minutes). The feeling may go away, but then come back, although it can be persistent.
- Discomfort in the upper body. People having a heart attack may feel pain or discomfort in the arms, neck, back, jaw, or stomach.
- Shortness of breath, which can occur with or without chest pain.
- Nausea and vomiting.
- Breaking out in cold sweat.
- Lightheadedness or fainting.
- Anxiety and a sense of impending doom.
Symptoms That are Less Likely to Indicate Heart Attack
The following symptoms are less likely to be due to heart attack:
- Sharp pain brought on by breathing in or when coughing.
- Pain that is mainly or only in the middle or lower abdomen.
- Pain that can be pinpointed with the tip of one finger.
- Pain that can be reproduced by moving or pressing on the chest wall or arms.
- Pain that is constant and lasts for hours (although no one should wait hours if they suspect they are having a heart attack).
- Pain that is very brief and lasts for a few seconds.
- Pain that spreads to the legs.
However, the presence of these symptoms does not necessarily rule out a serious heart event.
Silent Ischemia
Some people with severe coronary artery disease DO NOT have angina pain. This condition is known as silent ischemia. This is a dangerous condition because people have no warning signs of heart disease.
What to do When Symptoms Occur
If you are having chest pain or other symptoms that may indicate a heart attack, you should:
- Call 9-1-1 right away and wait for an ambulance. DO NOT attempt to drive yourself to the hospital.
- After you call 9-1-1, chew 1 adult-size (325 mg) or 4 baby (81 mg) non-coated aspirin. Be sure to tell the paramedics so an additional aspirin dose is not given.
- For people with angina, take one nitroglycerin dose as prescribed at the first onset of symptoms or as directed. Some people may be told to take up to three doses, 5 minutes apart. If symptoms DO NOT go away or worsen after the maximum number of tablets has been taken, call 9-1-1.
Diagnosis
When a person comes to the hospital with chest pain, the following diagnostic steps are usually taken to determine any heart problems and, if present, their severity:
- The patient or caretaker will report all symptoms so that a health care provider can rule out either a non-heart problem or possible other serious accompanying conditions.
- An electrocardiogram (ECG) reading is taken, recording the electrical activity of the heart. It is the key tool for determining if heart problems are causing chest pain. Paramedics sometimes perform an ECG in the ambulance on the way to the hospital.
- Blood tests showing elevated levels of certain factors (troponins and CK-MB) indicate heart damage. (The doctor will not wait for results, however, before administering treatment if a heart attack is strongly suspected. This is because all of these markers take some time from the onset of a heart attack to become abnormal.)
- Imaging tests, including echocardiogram and perfusion scintigraphy, may help rule out a heart attack if there is any question.
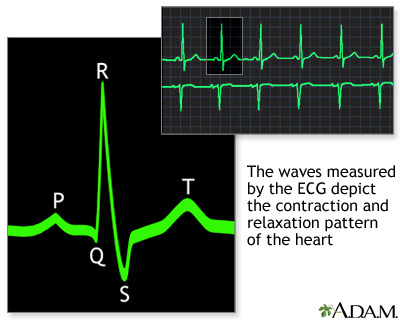
Electrocardiogram (ECG)
An electrocardiogram (ECG or EKG) measures and records the electrical activity of the heart. The waves measured by the ECG correspond to the contraction and relaxation pattern of the different parts of the heart. Specific waves seen on an ECG are named with letters:
- P. The P wave is associated with the contractions of the atria (the two chambers that receive blood from outside the heart).
- QRS. The QRS is a series of waves associated with ventricular contractions. (The ventricles are the two major pumping chambers in the heart.)
- T and U. These waves follow the ventricular contractions.
Doctors also use a term called the P-R interval, which is the time it takes for an electrical impulse to travel from the atria to the ventricles.
The most important wave patterns in diagnosing and determining treatment for a heart attack are called ST elevations and Q waves.
Elevated ST Segments: Heart Attack
Elevated ST segments are strong indicators of a heart attack in people with compatible symptoms and other indicators. They suggest that an artery to the heart is completely blocked and that the full thickness of the heart muscle is at risk. The kind of heart attack associated with these findings is referred to as either a Q-wave myocardial infarction or a STEMI.
However, ST-segment elevations DO NOT always mean the person has a heart attack. For example, inflammation in the sack around the heart (pericarditis) is another cause of ST-segment elevation.
Non-Elevated ST Segments: Stable Angina, Unstable Angina, and Non-ST Segment Elevation Myocardial Infarction
A significantly depressed ST segment may suggest some degree of coronary artery blockage and the presence of heart disease, even if there is no angina present. It occurs in about half of peoples with other signs of a heart event. This finding, however, is not very specific and can occur without narrowed coronary arteries. In such cases, laboratory tests are needed to determine the extent, if any, of heart damage.
In general, one of the following conditions may be present:
- Stable Angina is usually diagnosed in outpatients. People describe chest pain (or other symptoms noted above) that is predictable with certain activities or situations and resolves with rest.
- Unstable angina and NSTEMI (previously referred to as non Q-wave myocardial infarction) are more acutely serious conditions. People with unstable angina may have had stable angina before but it is now worse or comes with less activity or even at rest. They may have ECG changes, but blood tests DO NOT show markers for heart attack. With NSTEMI, the symptoms and signs may be similar, but the blood tests indicate a heart attack. People with unstable angina or NSTEMI are admitted to the hospital.
Echocardiogram
An echocardiogram is a non-invasive test that uses ultrasound images of the heart. Your doctor can see whether a part of your heart muscle has been damaged and is not moving normally. An echocardiogram may also be used as part of an exercise stress test, to detect the location and extent of heart muscle and other areas which may be "at risk," at the time of discharge or soon after you leave the hospital after a heart attack.
Radionuclide Imaging (Thallium Stress Test)
Radionuclide procedures use imaging techniques and computer analyses to plot and detect the passage of radioactive tracers through the region of the heart. Such tracing elements are typically given intravenously. Radionuclide imaging is useful for diagnosing and determining:
- Severity of unstable angina when less expensive diagnostic approaches are unavailable or unreliable.
- Severity of chronic coronary artery disease.
- Success of surgeries or other procedures for coronary artery disease.
- Whether a heart attack has occurred.
- The location and extent of heart muscle damage at the time of discharge or soon after the patient leaves the hospital after a heart attack.
- Areas at risk due to decreased blood flow with stress.
The procedure is non-invasive. It is a reliable measure of severe heart events and can help identify if damage has occurred from a heart attack. A radioactive isotope such as thallium (or technetium) is injected into the person's vein. The radioactive isotope attaches to red blood cells and passes through the heart in the circulating blood. The isotope can then be traced through the heart using special cameras called scanners.
The person is imaged while resting, then imaged again after an exercise stress test. Sometimes scans are done to evaluate if damaged heart muscle may recover if blood flow is improved. For these tests, images are obtained after a significant delay (up to 24 hours). This is called a myocardial "viability study."
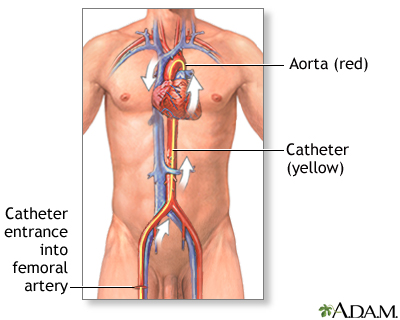
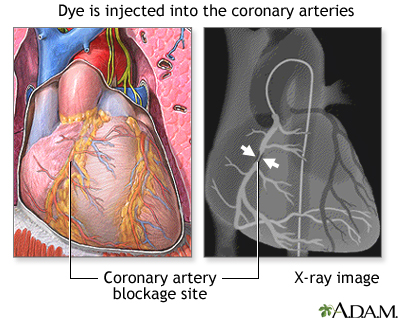
Angiography
Angiography is an invasive test. It is used when doctors require a detailed "road map" of coronary artery blockages. In the procedure:
- A narrow tube is inserted into an artery, usually in the leg or arm, and then threaded through the body to the coronary arteries.
- A dye (also called "contrast") is injected into the tube, and an x-ray records the flow of dye through the arteries.
- This process provides a map of the coronary circulation, revealing any blocked or narrowed areas.
Biological Markers
When heart cells become damaged, they release different enzymes and other molecules into the bloodstream. Elevated levels of such markers of heart damage in the blood may help diagnose a heart attack in people with severe chest pain and help determine treatment. Tests for these markers are often performed in the emergency room or hospital when a heart attack is suspected. Examples of such markers include the proteins creatine kinase myocardial band (CK-MB) and cardiac troponin T and I, which are released when the heart muscle is damaged. Troponins are the most specific biomarkers for diagnosing heart attack.
Troponins
The proteins cardiac troponin T and I are released when the heart muscle is damaged. Troponins are the most specific biomarkers for diagnosing heart attack. Cardiac troponin levels are normally so low they cannot be detected with most blood tests. Having normal troponin levels 12 hours after chest pain has started means a heart attack is unlikely, but does not rule out unstable angina.
Even a slight increase in the troponin level will often mean there has been some damage to the heart. Higher levels of troponin are a sign that a heart attack has occurred. Most people who have had a heart attack have increased troponin levels within 6 hours (3 to 12 hours). After 12 hours, almost everyone who has had a heart attack will have raised levels. Troponin levels may remain high for 1 to 2 weeks after a heart attack.
Increased troponin levels may also be due to:
- Abnormally fast heartbeat
- High blood pressure in lung arteries (pulmonary hypertension)
- Blockage of a lung artery by a blood clot, fat, or tumor cells (pulmonary embolus)
- Congestive heart failure
- Coronary artery spasm
- Inflammation of the heart muscle usually due to a virus (myocarditis)
- Prolonged exercise (for example, due to marathons or triathlons)
- Trauma that injures the heart, such as a car accident
- Weakening of the heart muscle (cardiomyopathy)
- Long-term kidney disease
Creatine kinase myocardial band (CK-MB)
CK-MB had been a standard marker for many years, but is not as accurate as troponin levels, because there are more conditions where elevated levels can appear in people without heart injury.
Treatment
Heart attack is usually treated by:
- Providing supportive treatments (oxygen, morphine) to relieve pain and stabilize the patient.
- When a completely blocked artery is suspected, opening up the artery as soon as possible (reperfusion therapy) by performing emergency angioplasty or using medicines that dissolve the clot (thrombolytics). Angioplasty may also be done less urgently in cases where an artery is not completely blocked, but is severely narrowed.
- Blocking further clotting (if possible), using an antiplatelet drug such as aspirin or clopidogrel (Plavix, generic), or other clot-fighting drugs (such as heparin, glycoprotein IIb/IIIa inhibitors, or bivalirudin).
- Helping the heart muscle and arteries work better by giving the person beta blockers, calcium channel blockers, or ACE inhibitor drugs.
- Controlling any arrhythmias (abnormal heart rhythms).
Immediate Treatments to Support the Patient
Oxygen
Oxygen is almost always administered right away, usually through a tube that sits in the nostrils.
Aspirin
The person is given aspirin if one was not taken at home.
Medications for Relieving Symptoms
- Nitroglycerin. Most people will receive nitroglycerin during and after a heart attack, usually under the tongue. Nitroglycerin decreases blood pressure and dilates (makes bigger) the blood vessels that feed the heart muscle, increasing blood flow. Nitroglycerin may be given intravenously in certain cases (recurrent angina, heart failure, or high blood pressure).
- Morphine. Morphine not only relieves pain and reduces anxiety but also relaxes blood vessels, aiding the circulation of blood and oxygen to the heart and lungs. Morphine can decrease blood pressure and slow down the heart. In people in whom such effects may worsen their heart attacks, other drugs may be used.
Opening the Arteries: Emergency Angioplasty or Thrombolytic Drugs
With a STEMI heart attack, a clot that has formed in a coronary artery that supplies oxygen to the heart muscle blocks it completely. Opening a clotted artery as quickly as possible is the best way to improve survival and limit the amount of heart muscle that is permanently damaged. Guidelines recommend that communities have emergency systems in place to ensure that heart attack patients are directed to appropriate medical centers equipped to treat them as quickly as possible.
The standard medical and surgical solutions for opening arteries are:
- Angioplasty (usually with stent placement), also called percutaneous coronary intervention (PCI), is the preferred emergency procedure for opening the arteries. Angioplasty should be performed promptly for patients with STEMI heart attack, preferably within 90 minutes of arriving at a hospital capable of performing the procedure. In most cases, a stent is placed in the artery to keep it open after the angioplasty. Guidelines recommend PCI for all people with STEMI attacks who have experienced symptom onset within the past 12 hours.
- Thrombolytics (clot-busting drugs) are the standard medications used to open the arteries. A thrombolytic drug should be given within 12 hours after the onset of symptoms. People who arrive at a hospital that is not equipped to perform PCI should receive clot-busting therapy within 30 minutes of arriving at the hospital and then are usually transferred to a PCI center without delay.
- Coronary artery bypass graft (CABG) surgery is sometimes used as an alternative to angioplasty. Referral for CABG depends on the location and number of blockages/narrowings as well as other factors such as the presence of heart failure, diabetes, and other medical problems. The timing of emergency CABG varies on the situation. It may be performed immediately or in a more delayed fashion.
Thrombolytics
Thrombolytic, also called clot-busting or fibrinolytic, drugs are recommended as alternatives to angioplasty. These drugs dissolve the clot, or thrombus, responsible for causing artery blockage and heart-muscle tissue death.
Generally speaking, thrombolysis is considered a good option for patients with full-thickness (STEMI) heart attacks when symptoms have been present for fewer than 12 hours. Ideally, these drugs should be given within 30 minutes of arriving at the hospital if angioplasty is not a viable option. Other situations where a clot-busting drug may be used include:
- When prolonged transport will be required
- If too long of a time will pass before a catheterization lab is available
Thrombolytics should be avoided or used with great caution in the following people:
- People older than 75 years
- When symptoms have lasted longer than 12 hours
- Pregnant women
- People who have experienced recent trauma (such as head injury) or invasive surgery
- People with active peptic ulcers
- People who have been given prolonged CPR
- Current users of anticoagulants
- People who have experienced any recent major bleeding
- People with a history of stroke
- People with uncontrolled high blood pressure, particularly when systolic pressure is higher than 180 mm Hg
Specific Thrombolytics
The standard thrombolytic drugs are recombinant tissue plasminogen activators or rt-PAs. They include alteplase (Activase) and reteplase (Retavase) as well as a newer drug tenecteplase (TNKase). Other types of drugs, such as a combination of an antiplatelet and anticoagulant, may also be given to prevent the clot from growing larger or any new clots from forming. Streptokinase, an older thrombolytic drug derived from Streptococcus bacteria, is also effective in dissolving blood clots, but can cause serious allergic reactions. Streptokinase is no longer used in the United States, but is still available in some regions of the world.
Thrombolytic Administration
The sooner that thrombolytic drugs are given after a heart attack begins, the better. The benefits of thrombolytics are highest within the first 3 hours. They can still help if given within 12 hours of a heart attack.
Complications
Hemorrhagic stroke, usually occurring during the first day, is the most serious complication of thrombolytic therapy, but fortunately it is rare.
Revascularization Procedures: Angioplasty and Bypass Surgery
PCI, also called angioplasty (usually done with stent placement), and CABG surgery are the standard procedures for dealing with narrowed or blocked arteries. These procedures help restore blood flow (perfusion). They are known as revascularization procedures:
- Emergency angioplasty/PCI is the standard procedure for heart attacks and should be performed preferably within 90 minutes of a heart attack. The benefits decline the longer it has been since the onset of a heart attack.
- Coronary bypass surgery is typically used as elective surgery for people with blocked arteries. It may be used after a heart attack if angioplasty or thrombolytics fail or are not appropriate, because too many blockages or blockages in certain areas are found. It is usually not performed for several days to allow recovery of the heart muscles.
Most people who meet the criteria for either thrombolytic drugs or angioplasty do better with angioplasty (although not all hospitals are equipped to do this procedure).
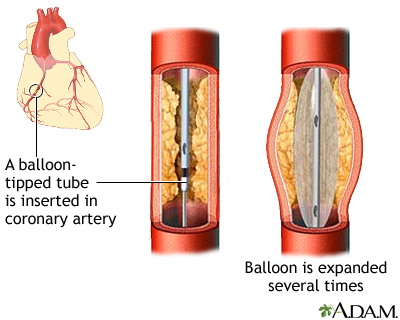
Angioplasty/PCI involves procedures such as percutaneous transluminal coronary angioplasty (PTCA) that help open the blocked artery. A typical angioplasty procedure involves the following steps:
- After the person receives some mild sedating medications, the cardiologist threads a narrow catheter (a tube) into the blocked vessel.
- The cardiologist opens the blocked vessel using balloon angioplasty, in which a tiny deflated balloon is passed through the catheter to the vessel.
- The balloon is inflated to compress the plaque against the walls of the artery, flattening it out so that blood can once again flow through the blood vessel freely.
- To keep the artery open afterwards doctors use a device called a coronary stent. An expandable metal mesh tube that is implanted during angioplasty at the site of the blockage. The stent may be bare metal or it may be coated with a drug that slowly releases medication. This medication decreases re-narrowing of the stented area.
- Once in place, the stent pushes against the wall of the artery to keep it open.
Complications occur in about 5% to 10% of people (most complications occur within the first day). Best results occur in hospital settings with experienced teams and backup. Women who have angioplasty after a heart attack have a higher risk of death than men.
Reclosure and Blockage During or After Angioplasty
Sudden narrowing or reclosure of the artery (stent thrombosis) can occur during or shortly after angioplasty, or even as long as a year or more after the procedure. When it occurs, the symptoms and signs are the same as those of a STEMI and usually require a repeat angioplasty procedure (a new stent is usually inserted within the prior one). This is a very serious and sometimes deadly occurrence.
Slow narrowing of a stent, which occurs because of new tissue growth in the wall of the artery and stent, is called "in-stent restenosis." With this condition, symptoms usually occur more gradually.
Drug-eluting stents, which are coated with everolimus, sirolimus, or paclitaxel, can help prevent restenosis, and reduce repeat procedures on the same area, although they do have a slightly higher risk of stent thrombosis.
Although all patients are prescribed aspirin and another antiplatelet medication (such as clopidogrel) for at least a year after a heart attack, those who have a stent placed must take both for at least a month for a bare metal stent and usually at least a year for a drug-eluting stent, unless directed by their cardiologist. This greatly reduces the risk of the stent closing suddenly. Clopidogrel, like aspirin, helps to prevent blood platelets from clumping together.
Prasugrel (Effient) is a newer antiplatelet drug that may be used as an alternative to clopidogrel for select patients with ACS who are undergoing angioplasty. It should not be used by patients who have had a previous stroke or transient ischemic attack. Another option for patients is the new antiplatelet drug ticagrelor (Brilinta). Like clopidogrel, these antiplatelets are taken in combination with aspirin.
If for some reason people cannot take a second antiplatelet along with aspirin after angioplasty and stenting for longer than 4 to 6 weeks, they should receive a bare metal stent instead of a drug-eluting stent.
Coronary Artery Bypass Graft Surgery (CABG)
CABG surgery is the alternative procedure to angioplasty for opening blocked arteries, particularly for people who have two or more blocked arteries. However, it is a very invasive procedure and requires a longer hospitalization and recovery period. In a CABG procedure:
- The chest is opened, and the blood is rerouted through a lung-heart machine.
- The heart is stopped during the procedure.
- Segments of veins or arteries taken from elsewhere in the person's body are fashioned into grafts, which are used to reroute the blood. The blood vessel grafts are placed in front of and beyond the blocked arteries, so the blood flows through the new vessels around the blockage.
Treatment for Patients in Shock or With Heart Failure
Severely ill people, particularly those with heart failure or who are in cardiogenic shock, will be monitored closely and stabilized. Oxygen is administered, and fluids are given or replaced when it is appropriate to either increase or reduce blood pressure. Such people may be given dopamine, dobutamine, or other powerful medications (or a combination). Other treatments such as mechanical assist devices (heart pumps) depend on the specific condition.
Heart failure
Intravenous furosemide or another diuretic may be administered to remove excess fluid from the lungs and other areas. People may also be given nitrates and ACE inhibitors, unless they have a severe drop in blood pressure or other conditions that preclude them. Clot-busting drugs or angioplasty may be appropriate.
Cardiogenic Shock
Cardiogenic shock is a dangerous condition that includes a drop in blood pressure and other abnormalities. Using a special long catheter, a procedure called intra-aortic balloon counterpulsation (IABP) can help people with cardiogenic shock around the time of revascularization. IABP involves inserting a catheter containing a long balloon, which is inflated and deflated within the artery to boost blood pressure and decrease the load on the heart. More powerful left ventricular assist devices that can provide more support may also be considered.
Treatment of Arrhythmias
An arrhythmia is a deviation from the heart's normal beating pattern caused when the heart muscle is deprived of oxygen.
Several different arrhythmias may occur during or after a heart attack. Some are less severe, but some can be deadly. Sometimes arrhythmias can cause the heart to beat very slowly and a pacemaker may be needed. Other arrhythmias may cause fast heart rhythms that can lead to sudden death.
Ventricular fibrillation
A lethal rhythm abnormality, in which the ventricles of the heart beat so rapidly that they DO NOT actually contract but quiver ineffectively. The pumping action necessary to keep blood circulating is lost.
Preventing Ventricular Fibrillation
People who develop ventricular fibrillation DO NOT always experience warning arrhythmias.
Preventive strategies include:
- Standard care of the heart attack performed promptly.
- Potassium and magnesium levels should be monitored and maintained.
- Beta blocker drugs may help prevent arrhythmias in certain people.
Treating Ventricular Fibrillation
Treatment strategies for ventricular fibrillation include:
- Defibrillators. People who develop ventricular arrhythmias are given electrical shocks with defibrillators to restore normal rhythms. In certain people, implantable cardioverter-defibrillators (ICDs) may prevent further arrhythmias in heart attack survivors of these events who are at risk for further arrhythmias.
- Antiarrhythmic Drugs. Antiarrhythmic drugs include lidocaine, procainamide, or amiodarone. Amiodarone or another antiarrhythmic drug may be used afterward to prevent future events.
Managing Other Arrhythmias
People with an arrhythmia called atrial fibrillation have a higher risk for stroke after a heart attack and are usually treated with anticoagulants such as warfarin (Coumadin, generic), dabigatran (Pradaxa), rivaroxaban (Xarelto), or apixaban (Eliquis). Other rhythm disturbances called bradyarrhythmias (very slow rhythm disturbances) frequently develop in association with a heart attack and may be treated with a drug called atropine or with a pacemaker.
Stroke
An in-depth report on the causes, diagnosis, treatment, and prevention of stroke.

| Read Article Now | Book Mark Article |
Medications
Aspirin and Other Anti-Clotting Drugs
Anti-clotting drugs that inhibit or break up blood clots are used at every stage of heart disease. Anti-clotting medications are generally classified as either antiplatelets or anticoagulants. Both antiplatelets and anticoagulants prevent blood clots from forming but they work in different ways:
- Antiplatelets prevent blood platelets from sticking together.
- Anticoagulants are "blood thinners" that reduce the ability of blood to clot.
All anti-clotting drugs increase the risk of bleeding, which can lead to dangerous situations, including stroke.
Appropriate anticlotting medications are started immediately in all patients. Such drugs are used with revascularization, and also as ongoing maintenance to prevent a heart attack.
Antiplatelet Drugs
These drugs inhibit blood platelets from sticking together, and therefore help to prevent clots. Platelets are very small disc-shaped blood cells that are important for blood clotting. Antiplatelet drugs include:
- Aspirin. Aspirin is an antiplatelet drug and should be taken immediately after a heart attack begins. It can be either swallowed or chewed, but chewing provides more rapid benefits. If the patient has not taken an aspirin at home, it will be given at the hospital. It is then continued daily (usually 81 mg/day). Using aspirin for heart attack patients has been shown to reduce mortality. It is the most common anti-clotting drug, and most people with heart disease are advised to take it daily in low doses on an ongoing basis. Aspirin can increase the risk for upper gastrointestinal bleeding. A combination drug containing aspirin and omeprazole (a proton pump inhibitor) was approved in 2016 by FDA for people who require secondary prevention of heart attack but who are at risk of developing gastric problems due to aspirin.
- Clopidogrel (Plavix, generic), a thienopyridine, is another type of antiplatelet drug. Clopidogrel is started either immediately before or right after angioplasty/PCI is performed. It is also begun after thrombolytic therapy. People who receive a drug-eluting stent should take clopidogrel along with aspirin usually for at least 1 year to reduce the risk of clots. Some people may need to take clopidogrel on an ongoing basis. Clopidogrel can increase the risk of upper gastrointestinal (GI) bleeding. Discuss with your doctor whether you should take a proton pump inhibitor (PPI). PPIs can reduce the risk of GI bleeding but some may also interfere with clopidogrel's anti-clotting effects.
- Prasugrel (Effient) is a thienopyridine that may be used instead of clopidogrel in people with ACS. It should not be used by people who have a history of stroke or transient ischemic attack.
- Ticagrelor (Brilinta) is another antiplatelet approved for people with ACS. It works differently than thienopyridines and must be taken twice a day. Cangrelor is the IV formulation of ticagrelor.
- Glycoprotein IIb/IIIa Inhibitors. These powerful antiplatelet drugs include abciximab (ReoPro), eptifibatide (Integrilin), and tirofiban (Aggrastat). They are administered intravenously in the hospital and are used around the time of revascularization procedures [angioplasty/PCI or coronary artery bypass graft (CABG) surgery].
Anticoagulant Drugs
Anticoagulants thin blood. They include:
- Heparin, which is usually started during or at the end of treatment with revascularization and may be continued for a few days.
- Other intravenous anticoagulants that may be given in the hospital, such as bivalirudin (Angiomax), fondaparinux (Arixtra), and enoxaparin (Lovenox).
- Warfarin (Coumadin, generic). dabigatran (Pradaxa), rivaroxaban (Xarelto), and apixaban (Eliquis) are other options for people with atrial fibrillation. (Only warfarin is used in people who have mechanical heart valves.)
- Some research indicates that the newer anticoagulants (dabigatran, rivaroxaban, apixaban) may pose a higher risk for bleeding in people with ACS than the older anticoagulant warfarin.
All of these drugs pose a risk for bleeding. In the event of life-threatening or uncontrolled bleeding due to anticoagulants, antidote drugs reversing the anticoagulant effect may sometimes be used. These include vitamin K (the antidote for warfarin), idarucizumab (Praxbind) for reversal of the direct thrombin inhibitor dabigatran, and coagulation factor Xa (Andexxa), a recently FDA approved drug reversing the effects of rivaroxaban and apixaban.
Beta Blockers
Beta blockers reduce the oxygen demand of the heart by slowing the heart rate and lowering pressure in the arteries. They are effective for reducing deaths from heart disease. Beta blockers are usually given to people early in their hospitalization, sometimes intravenously. People with heart failure or who are at risk of going into cardiogenic shock should not receive intravenous beta blockers. Long-term oral beta blocker therapy for people with symptomatic coronary artery disease, particularly after heart attacks, is recommended in most people.
Coronary artery disease
An in-depth report on the causes, diagnosis, treatment, and prevention of coronary artery disease (CAD).

| Read Article Now | Book Mark Article |
These drugs include propranolol (Inderal), carvedilol (Coreg), bisoprolol (Zebeta), acebutolol (Sectral), atenolol (Tenormin), labetalol (Normodyne, Trandate), metoprolol (Lopressor, Toprol-XL), and esmolol (Brevibloc). All of these drugs are available in generic form. The FDA is currently reviewing the safety and effectiveness of some generic forms of extended-release metoprolol.
Administration During a Heart Attack
The beta blocker metoprolol may be given orally or through an IV within the first few hours of a heart attack to reduce damage to the heart muscle.
Prevention After a Heart Attack
Beta blocker pills are also used on a long-term basis (as maintenance therapy) after a first heart attack to help prevent future heart attacks.
Side Effects
Although usually well-tolerated, beta blocker side effects can include fatigue, lethargy, vivid dreams and nightmares, depression, memory loss, and dizziness. They can lower HDL (good) cholesterol. Beta blockers are categorized as non-selective or selective. Non-selective beta blockers, such as carvedilol and propranolol, can narrow bronchial airways. Patients with asthma, emphysema, or chronic bronchitis, may need to avoid non-selective beta blockers.
People should not abruptly stop taking these drugs. The sudden withdrawal of beta blockers can rapidly increase heart rate and blood pressure. The doctor may want the person to slowly decrease the dose before stopping completely.
Statins
Anyone who has had a heart attack needs to take a statin drug to help lower cholesterol. After a heart attack, most people are asked to take more intensive doses.
The statin drugs approved in the United States are lovastatin (Mevacor, generic), pravastatin (Pravachol, generic), simvastatin (Zocor, generic), atorvastatin (Lipitor, generic), fluvastatin (Lescol), pitavastatin (Livalo), and rosuvastatin (Crestor).
People who cannot tolerate statin medications or those with very high cholesterol because of a genetic condition may be eligible for treatment with a special type of medication called PSK-9 inhibitors. Examples include alirocumab (Praluent) and evolocumab (Repatha).
Angiotensin Converting Enzyme Inhibitors
Angiotensin converting enzyme (ACE) inhibitors are important drugs for treating many people who have had a heart attack, particularly for people with and at risk for heart failure. ACE inhibitors should be given on the first day to such people with a heart attack, unless there are medical reasons for not taking them.
Almost all people admitted for ACS should receive ACE inhibitors if they have symptoms of heart failure or evidence of reduced left ventricular fraction on an echocardiogram. These drugs are also commonly used to treat high blood pressure (hypertension) and are recommended as first-line treatment for people with diabetes and kidney damage.
ACE inhibitors include captopril (Capoten), ramipril (Altace), enalapril (Vasotec), quinapril (Accupril), benazepril (Lotensin), perindopril (Aceon), and lisinopril (Prinivil, Zestril). All of these drugs are available in generic form.
Side Effects
Side effects of ACE inhibitors are uncommon but may include an irritating dry cough, excessive drops in blood pressure, and allergic reactions.
Calcium Channel Blockers
Calcium channel blockers may provide relief in people with unstable angina whose symptoms DO NOT respond to nitrates and beta blockers, or for people who are unable to take beta blockers, or for people who are still hypertensive (have high blood pressure) despite other medications.
Secondary Prevention
You can reduce your risk for a second heart attack by following secondary prevention measures. No one should be discharged from the hospital without these issues being addressed and appropriate medications prescribed. Lifestyle choices, particularly dietary factors, are equally important in preventing heart attacks.
Blood Pressure
Aim for a blood pressure of less than 130/90 mm Hg.
Cholesterol
Everyone who has had a heart attack should receive a prescription for a statin drug before being discharged from the hospital. It is also important to control dietary cholesterol by reducing intake of saturated fats to less than 7% of total calories. Increased omega-3 fatty acid consumption (by eating more fish or taking fish oil supplements) can help reduce triglyceride levels.
Control dietary cholesterol
An in-depth report on how to build the best diet for your heart's health.

| Read Article Now | Book Mark Article |
Diet
A heart-healthy diet emphasizes vegetables, fruits, and whole grains. Include low-fat dairy products, poultry, fish, beans, olive oil, and nuts. Limit sweets and red meats. Some research suggests that increasing fiber consumption (from specifically grains and cereals) may help attack survivors live longer. Evidence indicates that food is the best source for heart-protective antioxidants and minerals; multivitamins DO NOT seem to have much benefit for secondary, or primary, prevention. (According to the United States Preventive Services Task Force, there is insufficient evidence that regular use of multivitamin supplements helps prevent heart disease.)
Exercise
Although the AHA recommends 150 minutes of moderate activity or 75 minutes of vigorous activity per week for most people. People who already have cardiovascular disease should discuss an appropriate exercise regimen with their provider.
Weight Management
Exercise and diet are the foundations for weight management. Your body mass index (BMI) should be 18.5 to 24.8. Waist circumference is also an important measure of heart attack risk. Men's waist circumferences should be less than 40 inches (102 centimeters), while women's should be below 35 inches (89 centimeters). Guidelines recommend your doctor create an individualized weight loss plan for you if you are overweight or obese.
Smoking
It is essential to stop smoking and to avoid exposure to secondhand smoke.
Antiplatelet Drugs
Most people need to take low-dose aspirin (75 to 81 mg) on a regular daily basis after a heart attack. If you have had a drug-coated stent inserted, you must take another antiplatelet drug along with aspirin for at least 1 year following surgery. Most other people will also have a year of dual antiplatelet therapy prescribed.
The American Heart Association (AHA) recommends that people who have significant risk factors for atherosclerotic heart and vascular disease should take daily low-dose aspirin (if told to by their doctor) for primary prevention of heart attack or stroke. The AHA also recommends aspirin as secondary prevention for people who have already had a heart attack or stroke. For these people, the benefits of aspirin outweigh its risks, which include bleeding in the stomach and brain. People who DO NOT have current heart disease, high risk for heart disease, or a history of heart attack or stroke, should not take daily aspirin.
Other Drugs
Your doctor may recommend that you take an ACE inhibitor or beta blocker drug on an ongoing basis. It is also important to have an annual influenza ("flu") vaccination.
Rehabilitation
Cardiac rehabilitation is extremely important after a heart attack. A cardiac rehabilitation program is coordinated by a multidisciplinary team that includes cardiologists, cardiac nurses, nutritional counselors, exercise physiologists, and others. The goal of cardiac rehabilitation is to help the patient regain physical strength, improve heart and overall health, and reduce the chances of having another heart attack.
Cardiac rehabilitation typically takes place on site, at a hospital-affiliated facility. Services may be offered as individual sessions or group classes, depending on the type of rehabilitation therapy.
Cardiac rehabilitation begins with a comprehensive evaluation and patient assessment, which includes a physical exam and exercise tolerance test. Your healthcare team will evaluate your physical and emotional health, and any lifestyle issues that may affect your ability to manage your health. Based on this information, the team will design an individualized rehabilitation plan for you.
A cardiac rehabilitation plan may include:
- Supervised exercise program
- Nutritional counseling and weight management
- Education on disease management
- Behavioral and mental health counseling
- Stress management and relaxation training
Supervised Exercise
A supervised exercise program is an essential component of cardiac rehabilitation. Exercise therapy may include aerobic activity on a treadmill, stationary bike, rowing machine, or walking/jogging track, as well as strength training. Your cardiac rehab team will monitor your heart rate and rhythm, and gradually increase the intensity of your workout. You will also be given exercises to practice at home.
Nutritional Counseling
A nutritionist will review your eating habits and help you create dietary strategies that incorporate heart-healthy principles such as limiting saturated fats. The nutritionist may suggest following eating patterns such as the Mediterranean diet, which includes vegetables, fruits, fish, beans, nuts, and olive oil.
Weight Management
Exercise and diet are fundamental to weight control, but losing weight can be challenging for many patients. A cardiac rehab program may include a medically supervised weight loss program. Being overweight or obese significantly increases the risk for a future heart attack.
Stress Management
Coping with the physical, emotional, and lifestyle changes that follow a heart attack can be very stressful. Many cardiac rehabilitation programs offer instruction in relaxation techniques for stress management. Classes may include meditation, guided breathing, tai chi, yoga, or other forms of relaxation response.
Disease Management
Your program may offer educational classes and support groups on learning how to live and cope with heart disease.
Mental Health and Behavioral Counseling
Major depression occurs in many people who have ACS or who have had heart attacks. Studies suggest that depression is a major predictor for increased mortality in both women and men. (One reason may be that depressed patients are less likely to comply with their heart medications.)
Guidelines recommend depression screening for all people who have had a heart attack. Psychotherapeutic techniques, such as cognitive behavioral therapies, may be particularly helpful. For some people, certain types of antidepressant drugs may be appropriate.
Behavioral therapies can assist with unhealthy habits such as smoking. Quitting smoking is one of the most important steps to take for rehabilitation and prevention.
Sexual Counseling
Sexual activity can usually be safely resumed about a week after a heart attack, once a person can engage in mild-to-moderate exercise without experiencing cardiac symptoms. Ease into sexual activity gradually, starting with low-exertion acts (fondling, kissing).
The American Heart Association recommends sexual counseling for all patients and their partners who have experienced a cardiac event such as a heart attack. Discuss with your doctor how your medications may affect your sexual function, and be sure to report to your doctor any heart symptoms you experience during sex.
Resources
- National Heart, Lung, and Blood Institute -- www.nhlbi.nih.gov
- American College of Cardiology -- www.acc.org
- American Heart Association -- www.heart.org/en
- The National Coalition for Women with Heart Disease -- www.womenheart.org
References
American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions, O'Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78-e140. PMID: 23256914 pubmed.ncbi.nlm.nih.gov/23256914/.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. PMID: 25260718 pubmed.ncbi.nlm.nih.gov/25260718/.
Anderson JL, Morrow DA. Acute myocardial infarction. N Engl J Med. 2017;376(21):2053-2064. PMID: 28538121 pubmed.ncbi.nlm.nih.gov/28538121/.
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. PMID: 30879355 pubmed.ncbi.nlm.nih.gov/30879355/.
Bohula EA, Morrow DA. ST-elevation myocardial infarction: management. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 59.
Bonaca MP. Sabatine MS. The approach to the patient with chest pain. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 56.
Fleg JL, Forman DE, Berra K, et al. Secondary prevention of atherosclerotic cardiovascular disease in older adults: a scientific statement from the American Heart Association. Circulation. 2013;128(22):2422-2446. PMID: 24166575 pubmed.ncbi.nlm.nih.gov/24166575/.
Giugliano RP, Cannon CP, Braunwald E. Non ST-elevation acute coronary syndromes. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 60.
Grundy SM, Stone NJ; Guideline Writing Committee for the 2018 Cholesterol Guidelines. 2018 Cholesterol Clinical Practice Guidelines: Synopsis of the 2018 American Heart Association/American College of Cardiology/Multisociety Cholesterol Guideline. Ann Intern Med. 2019;170(11):779-783. PMID: 31132793 pubmed.ncbi.nlm.nih.gov/31132793/.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. PMID: 28886621 pubmed.ncbi.nlm.nih.gov/28886621/.
Jang JS, Spertus JA, Arnold SV, et al. Impact of multivessel revascularization on health status outcomes in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. J Am Coll Cardiol. 2015;66(19):2104-2113. PMID: 26541921 pubmed.ncbi.nlm.nih.gov/26541921/.
Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and The Obesity Society. J Am Coll Cardiol. 2014;129(25 Suppl 2):S102-S138. PMID: 24222017 pubmed.ncbi.nlm.nih.gov/24222017/.
Khan SU, Singh M, Valavoor S, et al. Dual Antiplatelet Therapy After Percutaneous Coronary Intervention and Drug-Eluting Stents: A Systematic Review and Network Meta-Analysis. Circulation. 2020;142(15):1425-1436. PMID: 32795096. pubmed.ncbi.nlm.nih.gov/32795096/.
Kulik A, Ruel M, Jneid H, et al. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation. 2015;131(10):927-964. PMID: 25679302 pubmed.ncbi.nlm.nih.gov/25679302/.
Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2016;134(10):e123-155. PMID: 27026020 pubmed.ncbi.nlm.nih.gov/27026020/.
Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2016;133(11):1135-1147. PMID: 26490017 pubmed.ncbi.nlm.nih.gov/26490017/.
Myerburg RJ, Goldberger JJ. Cardiac arrest and sudden cardiac death. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 42.
Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Nucl Cardiol. 2017;24(5):1759-1792. PMID: 28608183 pubmed.ncbi.nlm.nih.gov/28608183/.
Scirica BM, Libby P, Morrow DA. ST-elevation myocardial infarction: pathophysiology and clinical evolution. In: Zipes DP, Libby P, Bonow RO, Mann DL, Tomaselli GF, Braunwald E, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 58.
Steinke EE, Jaarsma T, Barnason SA, et al. Sexual counseling for individuals with cardiovascular disease and their partners: a consensus document from the American Heart Association and the ESC Council on Cardiovascular Nursing and Allied Professions (CCNAP). Circulation. 2013;128(18):2075-2096. PMID: 23897867 pubmed.ncbi.nlm.nih.gov/23897867/.
Valina C, Neumann FJ, Menichelli M, et al. Ticagrelor or Prasugrel in Patients With Non-ST-Segment Elevation Acute Coronary Syndromes. J Am Coll Cardiol. 2020;76(21):2436-2446. PMID: 33213722 pubmed.ncbi.nlm.nih.gov/33213722/.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2018;71(19):e127-e248. PMID: 29146535 pubmed.ncbi.nlm.nih.gov/29146535/.
Review Date: 4/14/2021
Reviewed By: Micaela Iantorno, MD MSc FAHA RPVI, Interventional Cardiologist at Mary Washington Hospital Center, Fredericksburg, VA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.