Partial knee replacement
Unicompartmental knee arthroplasty; Knee replacement - partial; Unicondylar knee replacement; Arthroplasty - unicompartmental knee; UKA; Minimally invasive partial knee replacement
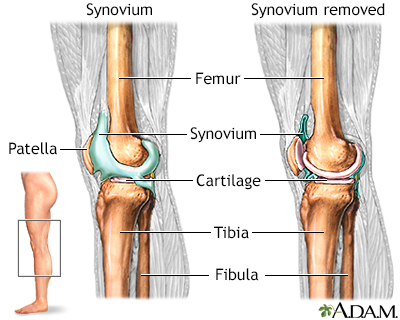
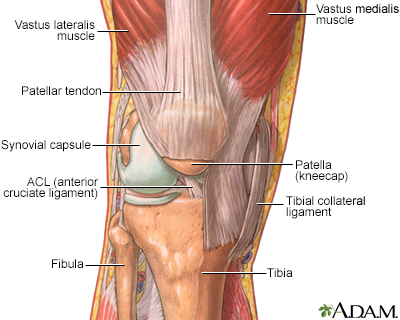
A partial knee replacement is surgery to replace only one part of a damaged knee. It can replace either the inside (medial) part, the outside (lateral) part, or the kneecap part of the knee.
Surgery to replace the whole knee joint is called total knee replacement.
Images
Presentation

Description
Partial knee replacement surgery removes damaged tissue and bone in the knee joint. It is done when arthritis is present in only part of the knee. The areas are replaced with an artificial implant, called a prosthetic. The rest of your knee is preserved. Partial knee replacements are most often done with smaller incisions, so there is less recovery time.
Before surgery, you will be given medicine that blocks pain (anesthesia). You will have one of two anesthesia types:
- General anesthesia. You will be asleep and pain-free during the procedure.
- Regional (spinal or epidural) anesthesia. You will be numb below your waist. You will also get medicines to make you relax or feel sleepy.
The surgeon will make a cut over your knee. This cut is about 3 to 5 inches (7.5 to 13 centimeters) long.
- Next, the surgeon looks at the entire knee joint. If there is damage to more than one part of your knee, you may need a total knee replacement. Most of the time this is not needed, because tests done before the procedure would have shown this damage.
- The damaged bone and tissue are removed.
- A part made from plastic and metal is placed into the knee.
- Once the part is in the proper place, it is attached with bone cement or fixated to the bone.
- The wound is closed with stitches or staples.
Why the Procedure Is Performed
The most common reason to have a partial knee joint replaced is to ease severe arthritis pain.
Your health care provider may suggest knee joint replacement if:
- You can't sleep through the night because of knee pain.
- Your knee pain prevents you from doing daily activities.
- Your knee pain has not gotten better with other treatments.
- Your knee pain limits your mobility
You will need to understand what surgery and recovery will be like.
Partial knee arthroplasty may be a good choice if you have arthritis in only one side or part of the knee and:
- You do not have very bad arthritis on the other side of the knee or under the kneecap.
- You have only minor deformity in the knee.
- You have good range of motion in your knee.
- The ligaments in your knee are stable.
However, most people with knee arthritis have a surgery called a total knee arthroplasty (TKA).
Knee replacement is most often done in people age 60 and older. Not all people can have a partial knee replacement. You may not be a good candidate if your condition is too severe. Also, your medical and physical condition may not allow you to have the procedure.
Risks
Risks for this surgery include:
- Blood clots
- Fluid buildup in the knee joint
- Failure of the replacement parts to attach to the knee
- Nerve and blood vessel damage
- Pain with kneeling
- Reflex sympathetic dystrophy (rare)
Before the Procedure
Always tell your surgeon which medicines you are taking, including herbs, supplements, and medicines bought without a prescription.
During the 2 weeks before your surgery:
- Prepare your home.
- Ask your surgeon which medicines you can still take on the day of your surgery.
- You may be asked to stop taking medicine that makes it harder for your blood to clot. These include aspirin, ibuprofen (Advil, Motrin), naproxen (Naprosyn, Aleve), blood thinners such as warfarin (Coumadin), and other drugs.
- You may need to stop taking any medicines that weaken your immune system, including Enbrel and methotrexate.
- If you have diabetes, heart disease, or other medical conditions, your surgeon will ask you to see the provider who treats you for these conditions.
- Tell your surgeon if you have been drinking a lot of alcohol (more than one or two drinks a day).
- If you smoke, you need to stop. Ask your providers for help. Smoking slows healing and recovery.
- Let your surgeon know if you get a cold, flu, fever, herpes breakout, or other illness before your surgery.
- You may want to visit a physical therapist before surgery to learn exercises that can help you recover.
- Practice using a cane, walker, crutches, or a wheelchair.
On the day of your surgery:
- You may be told not to drink or eat anything for 6 to 12 hours before the procedure.
- Take the medicines your surgeon told you to take with a sip of water.
- Your surgeon will tell you when to arrive at the hospital.
After the Procedure
You may be able to go home the same day or need to stay in the hospital for a day.
You can put your full weight on your knee right away.
After you return home, you should try to do what your surgeon tells you. This includes going to the bathroom or taking walks in the hallways with help. You will also need physical therapy to improve range of motion and strengthen the muscles around the knee.
Outlook (Prognosis)
Most people recover quickly and have much less pain than they did before surgery. People who have a partial knee replacement recover faster than those who have a total knee replacement.
Many people are able to walk without a cane or walker within 3 to 4 weeks after surgery. You will need physical therapy for 3 to 4 months.
Most forms of exercise are OK after surgery, including walking, swimming, tennis, golf, and biking. However, you should avoid high-impact activities such as jogging.
Partial knee replacement can have good results for some people. However, the unreplaced part of the knee can still degenerate and you may need a full knee replacement down the road. Partial inside or outside replacement has good outcomes for up to 10 years after surgery. Partial patella or patellofemoral replacement does not have as good long-term results as the partial inside or outside replacements. You should discuss with your surgeon whether you are a candidate for partial knee replacement and what the success rate is for your condition.
Related Information
Knee joint replacementArthritis
References
Althaus A, Long WJ, Vigdorchik JM. Robotic unicompartmental knee arthroplasty. In: Scott WN, ed. Insall & Scott Surgery of the Knee. 6th ed. Philadelphia, PA: Elsevier; 2018:chap 163.
Jevsevar DS. Treatment of osteoarthritis of the knee: evidence-based guideline, 2nd edition. J Am Acad Orthop Surg. 2013;21(9):571-576. PMID: 23996988 pubmed.ncbi.nlm.nih.gov/23996988/.
Mihalko WM. Arthroplasty of the knee. In: Azar FM, Beaty JH, eds. Campbell's Operative Orthopaedics. 14th ed. Philadelphia, PA: Elsevier; 2021:chap 7.
Weber KL, Jevsevar DS, McGrory BJ. AAOS Clinical Practice Guideline: surgical management of osteoarthritis of the knee: evidence-based guideline. J Am Acad Orthop Surg. 2016;24(8):e94-6. PMID: 27355287 pubmed.ncbi.nlm.nih.gov/27355287/.
BACK TO TOPReview Date: 8/12/2023
Reviewed By: C. Benjamin Ma, MD, Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery, San Francisco, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
