Corneal injury
Abrasion - corneal; Scratch - corneal; Eye pain - corneal
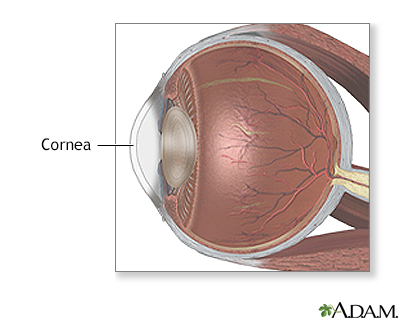
Corneal injury is a wound to the part of the eye known as the cornea. The cornea is the crystal clear (transparent) tissue that covers the front of the eye. It works with the lens of the eye to focus images on the retina.
Images
Animation

I Would Like to Learn About:
Causes
Injuries to the cornea are common.
Injuries to the outer surface may be due to:
- Abrasions -- Includes scratches or scrapes on the surface of the cornea
- Chemical injuries -- Caused by almost any fluid that gets into the eye
- Contact lens problems -- Overuse, poor fit, or sensitivity to contact lens care solutions
- Foreign bodies -- Exposure to something in the eye such as sand or dust
- Ultraviolet injuries -- Caused by sunlight, sun lamps, snow or water reflections, or arc-welding
Infections may also damage the cornea.
You are more likely to develop a corneal injury if you:
- Are exposed to sunlight or artificial ultraviolet light for long periods of time
- Have ill-fitting contact lenses or overuse your contact lenses
- Have very dry eyes
- Work in a dusty environment
- Use a hammer or power tools without wearing safety glasses
High-speed particles, such as chips from hammering metal on metal, may get stuck in the surface of the cornea. Rarely, they may penetrate deeper into the eye.
Symptoms
Symptoms include:
- Blurred vision
- Eye pain or stinging and burning in the eye
- Feeling like something is in your eye (may be caused by a scratch or something in your eye)
- Light sensitivity
- Redness of the eye
- Swollen eyelids
- Watery eyes or increased tearing
Exams and Tests
You will need to have a complete eye test. The health care provider may use eye drops containing fluorescein dye to help look for injuries.
Tests may include:
Treatment
First aid for eye emergencies:
- Do not try to remove an object that is stuck in your eye without professional medical help.
- If chemicals are splashed in the eye, immediately flush the eye with water for 15 minutes. The person should be quickly taken to the nearest emergency room.
Anyone with severe eye pain needs to be seen in an emergency care center or examined by an ophthalmologist right away.
Treatment for corneal injuries may involve:
- Removing foreign material from the eye
- Wearing an eye patch or temporary bandage contact lens
- Using eye drops or ointments prescribed by the doctor
- Not wearing contact lenses until the eye has healed
- Taking pain medicines
Outlook (Prognosis)
Most of the time, injuries that affect only the surface of the cornea heal very quickly with treatment. The eye should be back to normal within 2 days. For more serious injuries or when there may be delayed healing, placement of an amniotic membrane (from purified placental tissue) can be very helpful.
Injuries that penetrate the cornea are much more serious. The outcome depends on the specific injury.
When to Contact a Medical Professional
Contact your provider if the injury is not better after 2 days of treatment.
Prevention
Things you can do to prevent corneal injuries include:
- Wear safety goggles at all times when using hand or power tools or chemicals, during high impact sports, or during other activities where you may get an eye injury.
- Wear sunglasses that screen ultraviolet light when you are exposed to sunlight or are in the vicinity of arc welding. Wear this type of sunglasses even during the winter.
- Be careful when using household cleaners. Many household products contain strong chemicals. Drain and oven cleaners are very dangerous. They can lead to blindness if not used properly.
Related Information
Corneal ulcers and infectionsRetina
References
Dang DH, Riaz KM, Karamichos D. Treatment of non-infectious corneal injury: review of diagnostic agents, therapeutic medications, and future targets. Drugs. 2022;82(2):145-167. PMID: 35025078 pubmed.ncbi.nlm.nih.gov/35025078/.
Fowler GC. Corneal abrasions and removal of corneal or conjunctival foreign bodies. In: Fowler GC, ed. Pfenninger and Fowler's Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier; 2020:chap 200.
Guluma K, Lee JE. Ophthalmology. In: Walls RM, eds. Rosen's Emergency Medicine: Concepts and Clinical Practice. 10th ed. Philadelphia, PA: Elsevier; 2023:chap 57.
Knoop KJ, Dennis WR. Ophthalmologic procedures. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges' Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier; 2019:chap 62.
Rao NK, Goldstein MH. Acid and alkali burns. In: Yanoff M, Duker JS, eds. Ophthalmology. 4th ed. Philadelphia, PA: Elsevier; 2019:chap 4.26.
BACK TO TOPReview Date: 8/22/2022
Reviewed By: Franklin W. Lusby, MD, Ophthalmologist, Lusby Vision Institute, La Jolla, CA. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
