Cranial mononeuropathy VI
Abducens paralysis; Abducens palsy; Lateral rectus palsy; VIth nerve palsy; Cranial nerve VI palsy; Sixth nerve palsy; Neuropathy - sixth nerveCranial mononeuropathy VI is a nerve disorder. It affects the function of the sixth cranial (skull) nerve. As a result, the person may have double vision.
Causes
Cranial mononeuropathy VI is damage to the sixth cranial nerve. This nerve is also called the abducens nerve. It helps you move your eye sideways toward your temple.
Disorders of this nerve can occur with:
- Brain aneurysms
Aneurysms
An aneurysm is an abnormal widening or ballooning of a part of an artery due to weakness in the wall of the blood vessel.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Nerve damage from diabetes (diabetic neuropathy)
Diabetic neuropathy
Nerve damage that occurs in people with diabetes is called diabetic neuropathy. This condition is a complication of diabetes.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Gradenigo syndrome (which also causes discharge from the ear and eye pain)
- Tolosa-Hunt syndrome (inflammation of the area behind the eye)
- Increased or decreased pressure in the skull
- Infections (such as meningitis or sinusitis)
Meningitis
Meningitis is an infection of the membranes covering the brain and spinal cord. This covering is called the meninges.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleSinusitis
Sinusitis is present when the tissue lining the sinuses become swollen or inflamed. It occurs as the result of an inflammatory reaction or an infect...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Multiple sclerosis (MS), a disease that affects the brain and spinal cord
Multiple sclerosis
Multiple sclerosis (MS) is an autoimmune disease that affects the brain and spinal cord (central nervous system).
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Pregnancy
-
Stroke
Stroke
A stroke occurs when blood flow to a part of the brain stops. A stroke is sometimes called a "brain attack. " If blood flow is cut off for longer th...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Trauma (caused by head injury or accidentally during surgery)
- Tumors around or behind the eye
While rare, it can also be present at birth (congenital).
The exact cause of vaccination-related cranial nerve palsy in children is not known.
Because there are common nerve pathways through the skull, the same disorder that damages the sixth cranial nerve may affect other cranial nerves (such as the third or fourth cranial nerve).
Symptoms
When the sixth cranial nerve doesn't work properly, you can't turn your eye outward toward your ear. You can still move your eye up, down, and toward the nose, unless other nerves are affected.
Symptoms may include:
-
Double vision when looking to one side
Double vision
There are many types of eye problems and vision disturbances, such as: Halos Blurred vision (the loss of sharpness of vision and the inability to see...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article - Headaches
- Pain around the eye
Exams and Tests
Tests often show that one eye has trouble looking to the side while the other eye moves normally. An exam shows the eyes do not line up either at rest or when looking in the direction of the weak eye.
Your health care provider will do a complete exam to determine the possible effect on other parts of the nervous system. Depending on the suspected cause, you may need:
- Blood tests
- Head imaging study (such as an MRI or CT scan)
MRI
A head MRI (magnetic resonance imaging) is an imaging test that uses powerful magnets and radio waves to create pictures of the brain and surrounding...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark ArticleCT scan
A head computed tomography (CT) scan uses many x-rays to create pictures of the head, including the skull, brain, eye sockets, and sinuses.
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article -
Spinal tap (lumbar puncture)
Spinal tap
Cerebrospinal fluid (CSF) collection is a test to look at the fluid that surrounds the brain and spinal cord. CSF acts as a cushion, protecting the b...
 ImageRead Article Now Book Mark Article
ImageRead Article Now Book Mark Article
You may need to be referred to a doctor who specializes in vision problems related to the nervous system (neuro-ophthalmologist).
Treatment
If your provider diagnoses swelling or inflammation of, or around the nerve, medicines called corticosteroids may be used.
Sometimes, the condition disappears without treatment. If you have diabetes, you'll be advised to keep tight control of your blood sugar level.
Blood sugar level
A blood sugar test measures the amount of a sugar called glucose in a sample of your blood. Glucose is a major source of energy for most cells of the...

Your provider may prescribe an eye patch to relieve the double vision. The patch can be removed after the nerve heals.
Surgery or special glasses (prisms) may be advised if there is no recovery in 6 to 12 months.
Outlook (Prognosis)
Treating the cause may improve the condition. Recovery often occurs within 3 months in older adults who have hypertension or diabetes. There is less chance of recovery in case of complete paralysis of the sixth nerve. The chances of recovery are less in children than in adults in case of traumatic injury of the nerve. Recovery is usually complete in cases of benign sixth nerve palsy in childhood.
Possible Complications
Complications may include permanent vision changes.
When to Contact a Medical Professional
Contact your provider if you have double vision.
Prevention
There is no way to prevent this condition. People with diabetes may reduce the risk by controlling their blood sugar.
References
Olitsky SE, Marsh JD. Disorders of eye movement and alignment. In: Kliegman RM, St. Geme JW, Blum NJ, et al, eds. Nelson Textbook of Pediatrics. 22nd ed. Philadelphia, PA: Elsevier; 2025:chap 663.
Rucker JC, Seay MD. Cranial neuropathies. In: Jankovic J, Mazziotta JC, Pomeroy SL, Newman NJ, eds. Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Philadelphia, PA: Elsevier; 2022:chap 103.
Thurtell MJ, Rucker JC. Neuro-ophthalmology. In: Winn HR, ed. Youmans and Winn Neurological Surgery. 8th ed. Philadelphia, PA: Elsevier; 2023:chap 15.
Tamhankar MA. Eye movement disorders: third, fourth, and sixth nerve palsies and other causes of diplopia and ocular misalignment. In: Liu GT, Volpe NJ, Galetta SL, eds. Liu, Volpe, and Galetta's Neuro-Ophthalmology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 15.
-
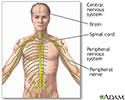
Central nervous system and peripheral nervous system - illustration
The central nervous system comprises the brain and spinal cord. The peripheral nervous system includes nerves outside the brain and spinal cord.
Central nervous system and peripheral nervous system
illustration
Review Date: 6/13/2024
Reviewed By: Joseph V. Campellone, MD, Department of Neurology, Cooper Medical School at Rowan University, Camden, NJ. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.