Thyroid cancer - papillary carcinoma
Papillary carcinoma of the thyroid; Papillary thyroid cancer; Papillary thyroid carcinoma
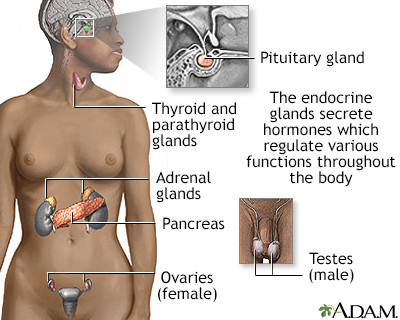
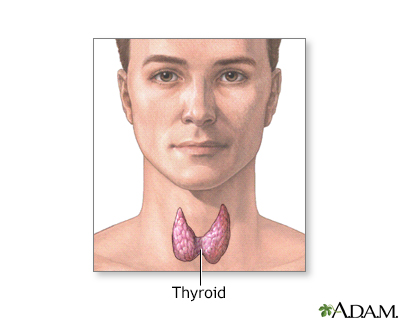
Papillary carcinoma of the thyroid is the most common cancer of the thyroid gland. The thyroid gland is located in front of the lower neck.
Images
I Would Like to Learn About:
Causes
About 85% of all thyroid cancers diagnosed in the United States are the papillary carcinoma type. It is more common in women than in men. It may occur in childhood, but is most often seen in adults between ages 20 and 60.
The cause of this cancer is not known. A genetic defect or family history of the disease may be a risk factor.
Radiation increases the risk for developing thyroid cancer. Exposure may occur from:
- High-dose external radiation treatments to the neck, especially during childhood, used to treat childhood cancer or some noncancerous childhood conditions
- Radiation exposure from nuclear plant disasters
Radiation given through a vein (through an IV) during medical tests and treatments does not increase the risk for developing thyroid cancer.
Symptoms
Thyroid cancer often begins as a small lump (nodule) in the thyroid gland.
While some small lumps may be cancer, most (90%) thyroid nodules are harmless and are not cancerous.
Most of the time, there are no other symptoms.
Exams and Tests
If you have a lump on your thyroid, your health care provider may order the following tests:
- Blood tests.
- Ultrasound of the thyroid gland and neck region.
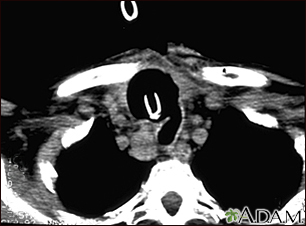
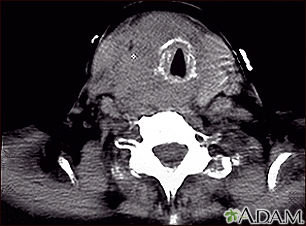
- CT scan of the neck or MRI to determine the size of the tumor.
- An examination of the airway with a fiberoptic scope (laryngoscopy) may show a paralyzed vocal cord.
- Fine needle aspiration biopsy (FNAB) to determine if the lump is cancerous. FNAB may be performed if the ultrasound shows that the lump is less than 1 centimeter.
Genetic testing may be done on the biopsy sample to see what genetic changes (mutations) may be present. Knowing this may help guide treatment recommendations.
Thyroid function tests are often normal in people with thyroid cancer.
Treatment
Thyroid cancer treatment may include:
- Surgery
- Radioactive iodine therapy
- Thyroid suppression therapy (thyroid hormone replacement therapy)
- External beam radiation therapy (EBRT)
Surgery is done to remove as much of the cancer as possible. The bigger the lump, the more of the thyroid gland must be removed. Often, the entire gland is taken out.
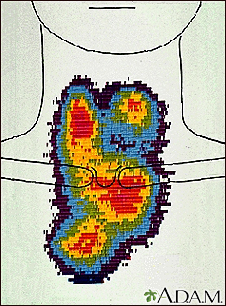
After the surgery, you may receive radioiodine therapy, which is often taken by mouth. This substance kills any remaining thyroid tissue. It also helps make medical images clearer, so doctors can see if there is any cancer left behind or if it comes back later.
Further management of your cancer will depend on many factors such as:
- Size of any tumor present
- Location of the tumor
- Growth rate of the tumor
- Symptoms you may have
- Your own preferences
If surgery is not an option, external radiation therapy can be useful.
After surgery or radioiodine therapy, you will need to take medicine called levothyroxine for the rest of your life. This replaces the hormone the thyroid would normally make.
Your provider will likely have you take a blood test every several months to check thyroid hormone levels. Other follow-up tests that may be done after treatment for thyroid cancer include:
- Ultrasound of the thyroid
- An imaging test called a radioactive iodine (I-131) uptake scan
- Repeat FNAB
Support Groups
You can ease the stress of illness by joining a cancer support group. Sharing with others who have common experiences and problems can help you not feel alone.
Outlook (Prognosis)
The survival rate for papillary thyroid cancer is excellent. More than 90% of adults with this cancer survive at least 10 to 20 years. The prognosis is better for people who are younger than 40 and for those with smaller tumors.
The following factors may decrease the survival rate:
- Older than 55 years of age
- Cancer that has spread to distant parts of the body
- Cancer that has spread to soft tissue around the thyroid
- Large tumor
Possible Complications
Complications include:
- Accidental removal of the parathyroid glands, which help regulate blood calcium levels
- Damage to the nerve that controls the vocal cords
- Spreading of cancer to lymph nodes (rare)
- Spreading of cancer to other sites (metastasis)
When to Contact a Medical Professional
Contact your provider if you have a lump in your neck.
Related Information
Thyroid cancerAnaplastic thyroid cancer
Thyroid cancer - medullary carcinoma
Cancer
Metastasis
References
NCCN Clinical Practice Guidelines in Oncology NCCN Guidelines) website. Thyroid carcinoma, Version 2.2024 - March 12, 2024. www.nccn.org/professionals/physician_gls/pdf/thyroid.pdf. Accessed May 10, 2024.
National Cancer Institute website. Thyroid cancer treatment (PDQ) - health provisional version. www.cancer.gov/cancertopics/pdq/treatment/thyroid/HealthProfessional. Updated April 11, 2024. Accessed May 3, 2024.
Pearce EN, Hollenberg AN. Thyroid. In: Goldman L, Cooney KA, eds. Goldman-Cecil Medicine. 27th ed. Philadelphia, PA: Elsevier; 2024:chap 207.
Sipos JA, Haugen BR. Papillary thyroid cancer. In: Randolph GW, ed. Surgery of the thyroid and parathyroid glands. 3rd ed. Philadelphia, PA: Elsevier; 2021:chap. 19.
Thompson LDR. Malignant neoplasms of the thyroid gland. In: Thompson LDR, Bishop JA, eds. Head and Neck Pathology. 3rd ed. Philadelphia, PA: Elsevier; 2019:chap 25.
BACK TO TOPReview Date: 3/31/2024
Reviewed By: Todd Gersten, MD, Hematology/Oncology, Florida Cancer Specialists & Research Institute, Wellington, FL. Review provided by VeriMed Healthcare Network. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.

Health Content Provider
06/01/2025
|
A.D.A.M., Inc. is accredited by URAC, for Health Content Provider (www.urac.org). URAC's accreditation program is an independent audit to verify that A.D.A.M. follows rigorous standards of quality and accountability. A.D.A.M. is among the first to achieve this important distinction for online health information and services. Learn more about A.D.A.M.'s editorial policy, editorial process and privacy policy. A.D.A.M. is also a founding member of Hi-Ethics. This site complied with the HONcode standard for trustworthy health information from 1995 to 2022, after which HON (Health On the Net, a not-for-profit organization that promoted transparent and reliable health information online) was discontinued. |
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 1997- 2024 A.D.A.M., a business unit of Ebix, Inc. Any duplication or distribution of the information contained herein is strictly prohibited.
