Depression - InDepth
Seasonal affective disorder - InDepth; Blues - InDepth; Gloom - InDepth; Sadness - InDepth; Melancholy - InDepthAn in-depth report on the causes, diagnosis, treatment, and prevention of depression.
- Highlights
What is Depression?
Depression is a mood disorder in which overwhelming feelings of sadness, loss of pleasure, guilt, and hopelessness interfere with daily life. People with depression also suffer from sleep problems, difficulty concentrating, fatigue and low energy, changes in appetite, and recurring thoughts of death or suicide.
In medical terms, depression is also referred to as major depression, major depressive disorder, or clinical depression.
American Psychiatric Association Treatment Guidelines
The American Psychiatric Association's guidelines for the treatment of people with major depressive disorder include:
- Exercise and other healthy behaviors (good nutrition, sleep hygiene, reducing use of tobacco, alcohol, and other harmful substances) are recommended for helping improve mood symptoms.
- Drug treatment is recommended for severe single and recurrent depressive episodes. Antidepressants are the main drugs used to treat depression.
- Individual or group therapies of various modalities can also be very helpful in the treatment of depression.
- Electroconvulsive therapy (ECT) may be helpful for people with treatment-resistant depression, particularly for people who have not responded to medication. Transcranial magnetic stimulation and vagus nerve stimulation are also possible options. Researchers are studying new types of brain stimulation treatments for depression.
- Introduction
Throughout life everyone experiences periods of temporary unhappiness and emotional pain. However, when sadness persists and impairs daily functioning, it may indicate a depressive disorder. Severity, duration, and the presence of other symptoms are the factors that distinguish normal sadness from clinical depression.
Clinical depression is classified as a mood disorder. The two main types are:
- Major depressive disorder, also called major depression
- Persistent depressive disorder (dysthymia), which is chronic but less severe major depression
Other depressive disorders include:
- Disruptive mood dysregulation disorder
- Premenstrual dysphoric disorder
- Depression due to substance abuse, medications, or a medical condition
Depression can also have different features or "specifiers." For example, depression may occur with:
- Anxious distress with anxiety-type symptoms such as feeling tense, restless, fearing something awful may happen, fearing losing control, or having difficulty concentrating because of worry.
- Mixed features, when elevated mood, inflated self-esteem, grandiosity, or racing speech or thoughts occur in a person who is mainly depressed. These are similar to the manic or hypomanic (milder) symptoms found in bipolar disorder. However, bipolar disorder is a separate illness. (Bipolar disorder can also have mixed features when depression occurs in someone who is mainly manic.)
- Atypical features, which are characterized by mood reactivity, the ability to experience improved mood in response to favorable experiences. Atypical features are accompanied by two or more symptoms such as sensitivity to rejection, hypersomnia (oversleeping), overeating, and leaden paralysis (feelings of heaviness in the arms and legs).
- Psychotic features, when delusions or hallucinations are present.
- Seasonal pattern, when major depression occurs regularly during a particular time of the year, such as the fall or winter. This is often referred to as seasonal affective disorder.
Depression is defined as a mood disorder, and there are several types.
Major depression is sometimes referred to as unipolar depression to distinguish it from bipolar depression, which is found in bipolar disorder. Bipolar disorder, formerly called manic-depression, is characterized by periods of depression alternating with episodes of excessive energy and activity (mania). Bipolar disorder is a separate mental illness not discussed in this report.
Major Depression
Major depression is also called major depressive disorder. In major depression, at least five of the symptoms listed below must occur nearly every day during a 2-week period, and they must represent a change from previous behavior or mood. Depressed mood or loss of interest or pleasure must be present. Symptoms include:
- Depressed mood on most days for most of each day -- irritability may be prominent in children and adolescents
- Total or very noticeable loss of interest or pleasure in activities most of the time
- Significant increases or decreases in appetite, weight, or both
- Sleep disorders, either insomnia or excessive sleepiness, nearly every day
- Feelings of agitation or a sense of intense slowness
- Loss of energy and a daily sense of tiredness
- Sense of guilt or worthlessness nearly all the time
- Inability to think or concentrate occurring nearly every day
- Recurrent thoughts of death or suicide
In addition, other criteria must be met:
- The symptoms listed above do not follow or accompany manic episodes (such as in bipolar disorder or other disorders).
- They impair important normal functions (such as work or personal relationships).
- They are not caused by drugs, alcohol, or other substances.
It can sometimes be difficult to distinguish the normal grief and anguish that comes with losing a loved one from the sadness and emptiness experienced with major depression. According to the American Psychiatric Association, the grief of loss usually decreases over time, and occurs in waves associated with thoughts of the deceased. In contrast, major depression is persistent and the sadness is not specific. However, bereavement can trigger a major depressive episode in some people.
Depression in Children
Symptoms for major depression in children can differ from those in adults and may include:
- An inability to enjoy favorite activities
- Persistent sadness
- Increased irritability
- Complaints of physical problems, such as headaches and stomach aches
- Poor performance in school
- Persistent boredom
- Low energy
- Poor concentration
- Changes in eating and/or sleeping patterns
Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder, or dysthymia, is a chronic depression characterized by many of the same symptoms that occur in major depression. Symptoms of dysthymia are less intense and last much longer, at least 2 years.
The symptoms of dysthymia have been described as a "veil of sadness" that covers most activities. Possibly because of the duration of the symptoms, people who suffer from chronic minor depression do not exhibit marked changes in mood or in daily functioning, although they have low energy, a general negativity, and a sense of dissatisfaction and hopelessness.
Other Types of Depressive Disorders
Disruptive Mood Dysregulation Disorder (DMDD)
DMDD is included with depressive disorders because children with DMDD are considered at risk of developing unipolar depression, and anxiety disorders, in adulthood.
The hallmark characteristic of DMDD is severe and recurrent temper outbursts that are far more extreme than typical "temper tantrums." These outbursts occur, on average, three or more times each week for a year or more. In between outbursts, children are persistently angry or irritable nearly every day. A diagnosis of DMDD requires that these outbursts be observed in at least two settings (at home, at school, or with peers).
A DMDD diagnosis is made for children between the ages of 6 to18 years; symptoms must have started before age 10. Although DMDD shares some similarities with bipolar disorder and oppositional defiant disorder, it is a different and separate illness. In fact, one of the APA's reasons for defining this condition was to prevent children from being misdiagnosed with bipolar disorder.
Premenstrual Dysphoric Disorder
Premenstrual dysphoric disorder is a type of depression associated with premenstrual syndrome, the days that occur before the onset of menstruation. Symptoms resolve within a few days after the period starts.
Symptoms include mood swings, increased irritability, anxiety, and depression. People also experience decreased interest in usual activities, difficulty concentrating, fatigue and lack of energy, overeating and food cravings, oversleeping or insomnia, and a general sense of feeling out of control. Physical symptoms such as breast tenderness, joint and muscle pain, and abdominal bloating are also common.
Seasonal Affective Disorder
Seasonal affective disorder (SAD) is technically a feature of depression rather than a type of depression. It is characterized by annual episodes of depression that follow a seasonal pattern.
For people who live in northern latitudes, SAD symptoms typically occur during fall or winter and improve in the spring or summer. Symptoms include fatigue and a tendency to overeat (particularly carbohydrates) and oversleep. Lack of exposure to sunlight may be a contributing factor.
- Causes
The causes of depression are not fully known. Depression is most likely due to a combination of genetic, biologic, and environmental factors.
Genetic Factors
Because depression often runs in families, it appears that a genetic component is involved. Studies have found that close relatives of people with depression are 2 to 6 times more likely to develop the condition than individuals without a family history.
Researchers studying genetic associations among psychiatric disorders have identified possible mutations that may link illnesses such as depression, bipolar disorder, and schizophrenia.
Biologic Factors
The basic biologic causes of depression are strongly linked to abnormalities in the delivery of certain key neurotransmitters (chemical messengers in the brain). These neurotransmitters include:
- Serotonin. Perhaps the most important neurotransmitter in depression is serotonin. Among other functions, it is important for feelings of well-being. Imbalances in the brain's serotonin levels can trigger depression and other mood disorders.
- Other Neurotransmitters. Other neurotransmitters possibly involved in depression include acetylcholine and catecholamines, a group of neurotransmitters that consists of dopamine, norepinephrine, and epinephrine (also called adrenaline).
Reproductive Hormones
In women, the female hormones estrogen and progesterone may play a role in depression.
Medications
Many prescription drugs can affect brain chemicals and trigger depression. These medications include certain types of drugs used for acne, high blood pressure, contraception, Parkinson disease, inflammation, epilepsy, hormone problems, cholesterol, gastrointestinal problems, and other conditions.
- Risk Factors
According to major surveys, major depressive disorder affects nearly 15 million Americans (about 7% of the adult population) in a given year. While depression is an illness that can affect anyone at any time in their life, the average age of onset is 32 (although adults ages 49 to 54 years are the age group with the highest rates of depression). Other major risk factors for depression include being female and living in poverty.
Depression in Women
Women of all ages, regardless of nationality, race, ethnicity, or socioeconomic level, have higher rates of depression than men. Women with depression are also at increased risk for accompanying eating disorders, such as anorexia nervosa and bulimia. While men with depression are more likely than women to die by suicide, women with depression are twice as likely to attempt suicide.
Some types of depression occur only in women, such as premenstrual dysphoric disorder, perinatal depression, and perimenopausal depression. The following factors may be involved:
- Puberty. While both boys and girls have similar rates of depression before puberty, girls have twice the risk for depression once they reach puberty. Hormonal and sociocultural factors may affect the development of depression in girls in this age group.
- Menstruation. Many women experience mood changes around the time of menstruation but a small percentage of women suffer from premenstrual dysphoric disorder, a specific type of depression that accompanies premenstrual syndrome.
- Pregnancy and Childbirth. Hormonal fluctuations and other physical changes that occur during and after pregnancy, especially when combined with relationship stress and anxiety, can contribute to depression. Postpartum depression is a severe depression (sometimes accompanied by psychotic symptoms) that occurs within the first year after giving birth. It may be due in part to the rapid decline of reproductive hormones that accompany childbirth. First-time mothers are particularly susceptible. Studies suggest that women are at greater risk for postpartum depression if they have a personal or family history of depression. Miscarriage also poses a risk for depression.
- Perimenopause and Menopause. Hormonal fluctuations that trigger depression can also occur when a woman is transitioning to menopause (perimenopause). Sleep disruptions are common during perimenopause and may contribute to depression. Once women pass into menopause, depressive symptoms usually resolve.
Depression in Men
Depression is not rare in men. In fact, white men over age 85 have the highest rates of suicide of any group. Men may be more likely than women to mask their depression by using alcohol. Some research suggests that depression in men is associated with the following indicators:
- Low tolerance to stress
- Behaviors such as "acting out" and being impulsive
- A history of alcohol or substance abuse
- A family history of depression, alcohol abuse, or suicide
Depression is less reported in the male population, but this may be caused by male tendencies to deny symptoms, avoid seeking help, and mask emotional disorders with behavior such as alcohol abuse.
Depression in Children and Adolescents
Depression can occur in children of all ages, but adolescents have the highest risk. Risk factors for depression in young people include having parents with depression, particularly if the mother is depressed. Early negative experiences and exposure to stress, neglect, or abuse also pose a risk for depression.
Adolescents who have depression are at significantly higher risk for substance abuse, recurring depression, and other emotional and mental health problems in adulthood.
Studies suggest that 3% to 5% of children and adolescents suffer from clinical depression, and 10% to 15% have some depressive symptoms.
Depression in Older Adults
About 1% to 5% of older adults suffer from depression. The rate increases significantly for those who have other chronic health problems, especially medical conditions that interfere with functional abilities, such as Alzheimer's, Parkinson disease, heart disease, and cancer. Depression may also occur in older people who require home healthcare or hospitalization. In addition, older people often have to contend with significant stressful life changes such as the loss of a spouse. Suicide risk is highest in the oldest age groups. Suicide in older people is the third-leading cause of death related to injury. Men account for the majority of these suicides, with divorced or widowed men at highest risk.
Medical Conditions Associated with Increased Risk of Depression
Severe or Chronic Medical Conditions
Any chronic or serious illness, such as diabetes or multiple sclerosis, can lead to depression. In addition, some medications taken for chronic medical problems (such as interferon or corticosteroids) may also contribute to depression.
Thyroid Disease
Hypothyroidism (a condition caused when the thyroid gland does not produce enough hormones) can be associated with depression. However, hypothyroidism may also be misdiagnosed as depression and go undetected.
Chronic Pain Conditions
Studies have reported a strong association between depression and headaches, including chronic tension-type and migraine. Fibromyalgia, arthritis, and other chronic pain syndromes are also associated with depression.
Stroke and Other Neurological Conditions
Having a stroke increases the risk of developing depression. Neurological conditions that impair movement or thinking, such as Parkinson or Huntington disease, are also associated with depression.
Heart Failure
People with heart failure or people who have suffered a heart attack are at increased risk for depression.
Insomnia and Sleep Disorders
Sleep abnormalities are a hallmark of depressive disorders, with many depressed people experiencing insomnia. Likewise, insomnia or other changes in waking and sleeping patterns can have significant effects on a person's mood, and perhaps worsen or prolong an underlying depression.
Other Risk Factors
Smoking
There is a significant association between cigarette smoking and a susceptibility to depression. People who are prone to depression face a 25% chance of becoming depressed when they quit smoking, and this increased risk persists for at least 6 months. What's more, depressed smokers find it difficult to stop smoking. Smokers with a history of depression are not encouraged to continue smoking, but rather to keep a close watch on recurrence of depressive symptoms if they do stop smoking.
- Complications
Depression is often chronic, with episodes of improvement followed by recurrence. About one-third of people with a single episode of major depression will have another episode within 1 year after discontinuing treatment, and more than one half will have a recurrence at some point in their lives. Depression is more likely to recur if the first episode was severe or prolonged, or if there have been prior recurrences.
Risk for Suicide
Depression increases the risk for suicide. In the United States, the risk for suicide in people with depression is around 20%, compared to just 1% in the general population. Suicidal preoccupation or threats of suicide should always be taken seriously. Suicide attempts are a major risk factor for subsequent successful suicide.
Suicide is the third most common cause of death among adolescents, and is one of the most devastating events that can happen to a family. Behavioral therapies, combined with antidepressants, may help prevent suicide. However, antidepressants can also raise the risk for suicidality (suicidal thoughts and behavior) in some young people, particularly those ages 18 to 24. [See "Suicidal Risk and Antidepressant Medications" in Drug Treatment Guidelines section in this report.]
Children, adolescents, and young adults who are prescribed antidepressant medication should be carefully monitored by both their parents and doctors, especially during the first few months of treatment, for any worsening of depression symptoms or changes in behavior.
The following are danger signs in young people:
- Withdrawal from friends
- Sudden decrease in school performance
- Loss of interest in activities that were previously found as pleasurable
- Unusual irritability
- Unusual changes in sleep or eating habits
Risk factors for suicide include a history of neglect or abuse, history of deliberate self-harm, a family member who committed suicide, access to firearms, and living in communities where there have been recent outbreaks of suicide among young people. A romantic break-up is often the trigger for a suicidal attempt in teenagers. Feeling connected with parents and family can help protect young people with depression from suicide.
Effect on Physical Health
Major depression in older people or in people with serious illness may reduce survival rates, even independently of any accompanying illness. Decreased physical activity and social involvement certainly play a role in the association between depression and illness severity.
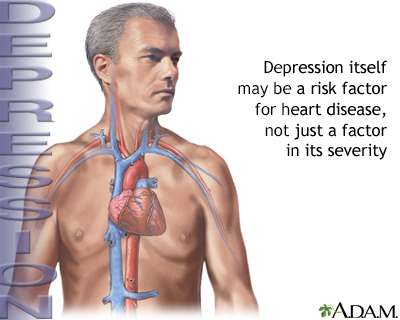
Heart Disease and Heart Attacks
Data suggest that depression itself may be a risk factor for heart disease as well as its increased severity. People with heart disease who are depressed tend to have more severe cardiac symptoms than those who are not depressed, and a poorer quality of life. Depression can worsen the prognosis of heart disease and increase the risk of death in people who have suffered a heart attack.
While the evidence is less conclusive, studies also indicate that depression in healthy people may increase the risk of developing heart disease. The more severe the depression, the greater the risk.
Studies are now showing that depression may contribute to poor outcomes for people with heart disease.
Obesity
People who are chronically depressed, especially adolescents, have a high risk for obesity. Conversely, obese people are about 25% more likely than non-obese people to develop depression or other mood disorders.
Mental Decline
Depression in older people is associated with a decline in mental functioning, regardless of the presence of dementia.
Cancer
Depression does not increase the risk for cancer, but like other chronic diseases, cancer increases the risk for depression. Cancer can also trigger depression by affecting chemicals in the brain. Sometimes, depressive symptoms can manifest before the cancer is diagnosed.
Impact on Daily Activities and Relationships
Effects of Parental Depression on Children
Depression in parents may increase the risk for childhood depression.
Effects on Marriage
People who suffer from psychiatric disorders tend to have higher divorce rates than healthy people. Spouses and partners of people with depression are themselves at higher risk for depression.
Effect on Work
Depression can adversely affect a person's ability to work and their normal work life. It significantly increases the risk for unemployment and lower-income.
Substance Abuse
Alcohol and Drug Abuse
Many people with major depression also struggle with alcohol or drug use problems. Studies on the connections between alcohol dependence and depression have still not resolved whether one causes the other or if they both share some common biologic factor.
Smoking
Depression is a well-known risk factor for smoking, and many people with major depression are nicotine dependent. Nicotine may stimulate receptors in the brain that improve mood in some people with depression.
- Diagnosis
A diagnosis of depression is based on symptoms meeting specific criteria. [See Introduction section of this report.] Many people who are depressed first seek help from their family doctors. Guidelines recommend that family doctors screen for depression in adults and adolescents (ages 12 to 18), as long as these doctors have appropriate systems in place to ensure accurate diagnosis, treatment, and follow-up of their people.
To check if you have depression, your doctor may ask questions such as:
- Over the past month, have you felt down, depressed or hopeless?
- Over the past month, have you felt little interest or pleasure in doing things?
Individuals who have certain factors might ask their doctor if they should be screened for depression. These factors include:
- Family or personal history of depression
- Multiple medical problems
- Physical symptoms that have no clear medical cause
- Chronic pain
- A need to visit the doctor more frequently than expected
Screening Tests
Screening tests such as the Beck Depression Inventory or the Hamilton Rating Scale consist of about 20 questions that assess depression. However, most mental health professionals generally diagnose depression based on symptoms and other criteria.
Symptoms of depression can vary depending on a person's cultural and ethnic background. For example, people from non-Western countries are more apt to report physical symptoms (such as headache, constipation, weakness, or back pain) related to the depression, rather than mood-related symptoms.
Ruling Out Other Conditions
Depression can sometimes be confused with other medical illnesses. Weight loss and fatigue, for example, accompany many health conditions but they can also occur with depression.
Depression may also be confused with other psychiatric disorders, such as bipolar disorder or attention-deficit hyperactivity disorder (ADHD). It is also common for people with depression to have other accompanying mental illnesses such as anxiety disorders, obsessive-compulsive disorder, or eating disorders such as anorexia nervosa or bulimia nervosa.
- Treatment
Depression is a treatable illness, with many therapeutic options available including psychotherapy, antidepressants, or both. In general, the treatment choice depends on the degree and type of depression and other accompanying conditions. Treatment approaches also depend on age, pregnancy status, and other individual factors.
In choosing treatment options, it is important for the person to be fully involved in the decision-making process.
People with Major Depression
Numerous studies support a combination of cognitive behavioral therapy (CBT) plus antidepressants, typically a selective serotonin reuptake inhibitor (SSRI) or serotonin norepinephrine reuptake inhibitor (SNRI). Although some people may feel better after taking antidepressants for a few weeks, most people need to take medication for at least 4 to 9 months to ensure a full response and to prevent depression from recurring. Research indicates that people respond better to medications when drug therapy is combined with CBT. Exercise may also help relieve depressive symptoms.
People with Treatment-Resistant Depression
For people with severe depression who are not helped by SSRIs or SNRIs, other types of antidepressants are available. Sometimes switching the antidepressant or combining two antidepressants with different mechanisms of action can help. Sometimes an atypical antipsychotic drug may be given in combination with an antidepressant for people with severe major depressive disorder. Atypical antipsychotics can have serious side effects, so their potential benefits must be weighed against their potential risks.
Brain stimulation techniques, such as electroconvulsive therapy (ECT), are options for treatment-resistant depression. Experimental procedures, such as repetitive transcranial magnetic stimulation and vagus nerve stimulation, may be helpful. Researchers are also investigating new types of drugs (such as ketamine), which may provide rapid, if temporary, improvement. In general, the more treatment strategies that people need, the less likely they are to recover completely from depression.
People with Minor Depression
People with minor depression (fewer than 5 symptoms that persist for fewer than 2 years) may respond well to watchful waiting to see if antidepressants are necessary. Counseling or cognitive behavioral therapy may be helpful, as is regular exercise.
People with Depression and Other Psychiatric Problems
Other psychiatric problems often coexist with depression. If people also suffer from anxiety, treating the depression first often relieves both problems. Research suggests that psychological treatment of insomnia may help boost the effectiveness of depression treatment in people who suffer from both conditions. More severe psychiatric problems, such as bipolar disorder or schizophrenia, require specialized treatments.
People with Depression and Medical Conditions
Depression can worsen many medical conditions and may even increase mortality rates from some disorders, such as heart attack and stroke. Depression should be aggressively treated in anyone with a serious medical problem.
People with Depression and Substance Abuse Problems
Treating depression in people who abuse alcohol or drugs is important and can sometimes help people quit. Likewise, addressing substance abuse is important for treatment of depression.
Choosing a Therapist
Most people with depression can be treated in an office setting by a psychiatrist, psychologist, or a therapist. In some cases, the depression may be serious enough to warrant hospitalization to provide protection from further deterioration or self-harm.
Health professionals who can prescribe antidepressants include:
- Doctors, including psychiatrists
- Nurse practitioners, including psychiatric and mental health nurse practitioners
Although other mental health professionals cannot prescribe drugs, most psychotherapists have arrangements with a psychiatrist for providing medications to their people. In general, mental health therapists are categorized by their educational training:
- Clinical psychologists have received a PhD, including several years of supervised clinical experience.
- Clinical social workers have received a master's or doctoral degree in social work (MSW or DSW) and several years of supervised clinical experience in mental health services.
Tips for selecting a therapist:
- People can locate a mental health professional in their area by asking their primary care doctor for a referral or by contacting a mental health organization. [See Resources section of this report.]
- People should describe problems briefly but specifically over the phone to any prospective therapist to get a sense of whether they will suit their needs.
- People should not be shy about considering a change in their therapist if they lack confidence in their current one.
Treating Depression During and After Pregnancy
Up to one-quarter of women experience depressive symptoms during pregnancy, and some women develop full-blown postpartum depression following delivery. Although a mother's depression during and after pregnancy can have serious effects on her child, researchers are still trying to determine the best methods for preventing and treating pregnancy-related depression.
The American College of Obstetricians and Gynecologists (ACOG) recommends that pregnant women with depression receive care from a multidisciplinary team that includes the person's obstetrician, primary care physician, and mental health clinician. Any woman who has suicidal or psychotic symptoms during depression should immediately seek treatment from a psychiatrist.
The use of antidepressants during pregnancy is controversial, especially for women with major depression who regularly take antidepressant medication. Most doctors advise women to avoid, if possible, any medications during pregnancy and nursing. But women with depression who stop taking antidepressants during pregnancy may be likely to have a relapse of depression, which can have negative consequences for prenatal care and subsequent mother-child bonding. The risks for negative outcomes are highest when depression occurs during the late second or early third trimester. Depression during pregnancy may also increase the risk of developing postpartum depression.
ACOG and the American Psychiatric Association (APA) recommend that women who are pregnant or thinking about becoming pregnant should not stop taking antidepressants without first talking to their doctors. Women who have mild or no depressive symptoms for at least 6 months before becoming pregnant may be able to taper off or discontinue antidepressant medication, under supervision of their doctor. Stopping medication may be more difficult for women with a history of severe recurrent depression. Psychotherapy (preferably cognitive behavioral therapy or interpersonal therapy) may be helpful in addition to, or in replacement of, antidepressant medication. Electroconvulsive therapy (ECT) may be an option for pregnant women with severe depression.
Studies have been inconsistent as to whether serotonin reuptake inhibitors (SSRIs) drugs increase the risk for birth defects. In general, the risks appear to be low, but doctors are still not sure. There is evidence that paroxetine (Paxil, generic) may cause major birth defects, including heart abnormalities, if taken during the first trimester of pregnancy. However, these findings have not been confirmed. Some studies have indicated that sertraline (Zoloft, generic) and citalopram (Celexa, generic) may also increase the risk of heart defects. The FDA has recently updated the public on the use of SSRIs by pregnant women and the potential for development of a rare heart and lung condition called persistent pulmonary hypertension of the newborn (PPHN). Due to conflicting data, the FDA advises health care providers to continue their current practice of treating depression in pregnancy.
SSRIs, and most tricyclic antidepressants, are considered safe to use during breastfeeding but more research is needed to clarify the effects of SSRI on infant and child development. [For more information, see "Selective Serotonin-Reuptake Inhibitors (SSRIs)" in Medications section.]
In terms of non-drug treatment of postpartum depression, doctors recommend that women with signs of postpartum depression receive intensive and individualized psychotherapy within a month after giving birth.
Treating Depression in Older Adults
Many doctors recommend only psychotherapy for older people with mild depression because antidepressants do not seem to add much benefit for these people. In many older people, a regular exercise program may be sufficient to improve mood. The use of antidepressants in older adults is problematic:
- Tricyclics are as effective as and less expensive than SSRIs, but they have more side effects. Specifically, they pose a higher risk for adverse effects on the heart and possibly the lungs. They also increase the risk for falling. (The older tricyclics, such as amitriptyline and imipramine, have other severe side effects in older adults.)
- SSRIs have fewer side effects than tricyclics. However, SSRIs may not pose any lower risk for falls than the older tricyclic antidepressants. In addition, researchers are investigating whether SSRIs are associated with an increased rate of osteoporosis ("thin bones") and hip fractures in older adults.
Treating Depression in Children and Adolescents
Studies suggest that when children or adolescents are treated for depression, most recover. Still, up to one-half of these young people have a recurrence of depression within 2 years of their first episode of depression.
It is important to recognize that childhood depression differs from adult depression and that children may respond differently than adults to antidepressant medication. These differences are due to childhood brain development processes as well as age-related differences in drug metabolism. Children may experience medication side effects not seen in adults, and some antidepressants that are effective for adults may not work for children.
Mild-to-Moderate Depression
The pediatrician may want to monitor a child with mild depression for 6 to 8 weeks before deciding whether to prescribe psychotherapy, antidepressant medication, or a referral to a mental health professional. Once medication has been started, the doctor will decide if the dosage needs to be increased after another 6 to 8 weeks. Medication may need to be continued for 1 year after the symptoms have resolved, and the doctor should continue to monitor the child on a monthly basis for 6 months after full remission of depression. For psychotherapy, cognitive therapy may be the best approach for children and adolescents with depression. Other types of psychotherapy, such as family therapy and supportive therapy, may also be effective.
Severe Depression
The American Academy of Child and Adolescent Psychiatry recommends an SSRI antidepressant for children and adolescents with very severe depression that does not respond to psychotherapy. Tricyclic antidepressants do not tend to help adolescents and children and these drugs have many side effects. MAOIs are also not commonly prescribed.
Fluoxetine (Prozac, generic) and escitalopram (Lexapro, generic) are the only SSRIs approved by the FDA for adolescents (ages 12 to 17), and fluoxetine is the only antidepressant approved for children age 8 and older. The FDA strongly advises against the use of some specific SSRIs, such as paroxetine (Paxil, generic), due to concerns about an increased risk for suicidal behavior as well as the lack of any evidence supporting the drug's efficacy in pediatric people. Some recent research indicates that the overall benefits of antidepressants for children and adolescents may outweigh the risks for suicidal behavior. For optimal results, SSRIs should be combined with either cognitive behavioral or interpersonal psychotherapy.
Due to potential suicide risks, children and adolescents should be monitored regularly during the initial months of antidepressant treatment. [For more detailed information, see "Suicide Risk and Antidepressant Medications" in Drug Treatment Guidelines section of this report.]
The American Psychiatric Association advises that while atypical antipsychotics are appropriate for treating conditions such as pediatric schizophrenia and bipolar disorder, they should not be routinely prescribed to children and adolescents for non-psychotic diagnoses. Atypical antipsychotics can cause serious harm in children, including weight gain, movement disorders, diabetes and other metabolic problems, and heart damage.
- Antidepressant Guidelines
Major Classes of Antidepressants and General Treatment Guidelines
Major classes of antidepressants include:
- Selective serotonin-reuptake inhibitors (SSRIs). These drugs have become the standard antidepressants. They target the brain chemical (neurotransmitter) serotonin. They can be effective and usually have moderate side effects.
- Other neurotransmitter inhibitors. These drugs target neurotransmitters other than or in addition to serotonin, such as norepinephrine. Many are proving to be effective in people who do not respond to standard antidepressants or in specific people, such as smokers who want to quit or people with chronic pain.
- Tricyclic antidepressants (TCAs). These drugs are effective but can have severe adverse effects, particularly in older people.
- Monoamine oxidase inhibitors (MAOIs). These drugs include newer selective MAOIs. MAOIs are very effective for some types of depression, but can have severe side effects and require restrictive dietary rules and care to avoid drug interactions.
All of these drugs appear to work equally well, although they may vary in terms of side effects. Your doctor will select an antidepressant based on side effects, cost, and your personal preference.
Approach and Duration of Initial Treatment
The guidelines for the duration of an initial antidepressant regimen are generally:
- People should start at a low dose, which is slowly increased as needed over a period of days to weeks.
- People should see their doctor every 1 to 2 weeks until substantial improvement occurs. It may take 4 to 8 weeks before a person experiences the effects of any antidepressant.
- Side effects usually diminish within 1 to 4 weeks. (Exceptions may be weight gain and sexual dysfunction.)
- If no improvement occurs within 6 to 8 weeks of starting drug treatment, the doctor may either increase the dosage or switch to an alternative drug. If one medication fails, another has a good chance of being helpful. In general, the fewer drug treatment strategies required, the better a person's chances of recovering completely from depression. People who become symptom-free have the best chance for complete recovery compared to people whose symptoms merely improve.
- In general, people should continue taking antidepressants for at least 4 to 9 months after symptom relief to help prevent relapse. People who have had at least 2 episodes of depression may need to continue drug treatment for longer than 9 months. (People who improve within 2 weeks of taking medications may not require lengthy treatment.)
Treating Recurrence
Relapse and recurrence of depression are very common. About one-third of people will relapse after a first episode within a year of ending treatment, and more than one half will experience a recurring bout of depression at some point during their lives. Among those at highest risk for early relapse and who may require ongoing antidepressants are:
- People with at least two episodes of major depression or major depression that lasts for 2 years or longer before initial treatment.
- People who continue to have low-level depression for 7 months after starting antidepressant treatments.
- People may need maintenance therapy. The American Psychiatric Association recommends considering maintenance therapy for people who have risk factors for depression recurrence. People who have experienced more than three prior depressive episodes, or who have chronic illnesses, should definitely be given maintenance therapy. Doctors disagree, however, on the optimal length or the appropriate dosage of maintenance therapy.
There is no risk for addiction with current antidepressants, and many of the common antidepressants, including most standard SSRIs, have been proven safe when taken for a number of years.
Common Side Effects of Most Antidepressants
No matter how well a drug treats depression, the ability of people to tolerate its side effects strongly influences their compliance with therapy. Side effects can be avoided or moderated if a regimen is started at low doses and built up over time. Although specific side effects are discussed under individual drugs, there are a few that are common to many of them:
- Sexual dysfunction is a common side effect of many of the standard antidepressants and some of the newer drugs. Some antidepressants, such as bupropion (Wellbutrin, generic), do not pose as high a risk for this problem. In men, PDE5 inhibitor drugs [sildenafil (Viagra), vardenafil (Levitra), tadalafil (Cialis), avanafil (Stendra)], may help improve sexual function. However, they do not increase the sex drive (libido). No specific therapy currently exists for treatment of antidepressant-induced sexual dysfunction in women.
- An increased risk of oral health problems caused by dry mouth is associated with long-term use of many antidepressants, particularly tricyclics. People can increase salivation by chewing gum, using saliva substitutes, and rinsing the mouth frequently.
- Virtually all antidepressants have complicated interactions with other drugs; some are very important. People should inform the doctor of any drugs they are taking, including over-the-counter medications and herbal remedies.
- Nearly all antidepressants are metabolized in the liver, so anyone with liver problems should use them with caution.
- Abrupt withdrawal from many antidepressants can produce severe side effects; no antidepressant should be stopped abruptly without consultation with a doctor. To avoid withdrawal symptoms, it is best to gradually taper off antidepressants rather than discontinue them abruptly.
Suicide Risk and Antidepressant Medications
In recent years, there has been concern that SSRI antidepressants can increase the risk for suicidal behavior. Of particular concern is a greater risk for suicide in young people taking these medications. While depression is itself the major risk factor for suicide, and antidepressant medication may revitalize suicidal attempts in people who were too despondent before treatment to make the effort, evidence suggests that in some cases the medication itself can cause suicidal thoughts and behavior (suicidality). Paroxetine (Paxil, generic) appears to have the strongest association with increased suicidal risk, particularly in younger adults.
In the United States, all antidepressant medications now carry "black box" warnings on their prescribing label explaining the association between antidepressant use and increased risk for suicidality in children, adolescents, and young adults ages 18 to 24, especially during the first few months of treatment. The FDA's data do not show an increased risk for suicidality in adults older than age 24. Adults age 65 years and older taking antidepressants have a decreased risk for suicidality.
The FDA recommends that caregivers monitor children, adolescents, and young adults being treated with antidepressants for sudden behavioral changes, and immediately notify their doctor if such changes occur. These behavioral signs include:
- Agitation
- Irritability
- Anxiety
- Panic attacks
- Insomnia
- Aggressiveness
- Impulsivity
- Hyperactivity in actions and speech
- Worsening of depression
- Increased thoughts of suicide
The FDA's guidelines for medication usage also recommend that all people see their doctors regularly after initiating drug treatment. The recommended schedule is:
- Once per week for 4 weeks (1st month).
- Every 2 weeks for the next month (2nd month).
- At the end of week 12 following the start of drug treatment (3rd month).
- More frequently if changes in mood or behavior occur.
- People should also be closely monitored if their drug dosage is changed.
People should immediately contact their doctor if depression symptoms worsen or if suicidal thoughts or behavior increase.
- Medications
Selective Serotonin-Reuptake Inhibitors (SSRIs)
Selective serotonin-reuptake inhibitors (SSRIs) are the first-line treatment for major depression. They work by increasing levels of serotonin in the brain. Because they act specifically on serotonin, SSRIs have fewer side effects than older antidepressants, which have more widespread effects in the body.
SSRI Brands
SSRIs include fluoxetine (Prozac, generic), sertraline (Zoloft, generic), paroxetine (Paxil, generic), fluvoxamine (Luvox, generic), citalopram (Celexa, generic), and escitalopram (Lexapro, generic). There do not appear to be significant differences among SSRI brands in effectiveness, although individual drugs may have different side effects or benefits for specific people.
At this time, fluoxetine and escitalopram are the only SSRI antidepressants approved for treatment of major depressive disorder in adolescents (ages 12 to 17). Fluoxetine is also approved for children age 8 and older.
New SSRIs
In recent years, the FDA has approved vortioxetine (Trintellix) that represents a new type of SSRI. This drug acts like an SSRI but has additional effects, not completely understood, on other serotonin 5-HT receptors in the brain. These new types of SSRIs are approved for treatment of major depression in adults.
Candidates for SSRIs
SSRIs appear to best help people with the following conditions:
- Moderate or severe major depression.
- Persistent depression (dysthymia).
- Premenstrual dysphoric disorder (PMDD). A repackaged form of fluoxetine (Sarafem) is specifically approved for PMDD. Other SSRIs and newer antidepressants may also be helpful.
- Seasonal affective disorder.
- Anxiety disorders.
- Bulimia nervosa.
Duration of Effectiveness and Use
SSRIs take, on average, 2 to 4 weeks to be effective. They may take even longer, up to 12 weeks, in older people and in those with dysthymia. By 14 weeks, depression should be in remission in those who respond to the drugs. Unfortunately, recurrence is common once the drugs are stopped. Studies indicate that the standard SSRIs are generally safe to be taken for the long-term, although it is still unclear which people most benefit from on-going medication. Some doctors recommend withdrawing from medication after a year. If depression recurs, then people should go back on the antidepressant.
Side Effects of SSRIs
Side effects may include:
- Nausea and gastrointestinal (GI) symptoms, which usually wear off over time.
- Insomnia or drowsiness, depending on the drug.
- Agitation and nervousness.
- Dry mouth.
- Headache.
- Heart palpitations (see below for citalopram heart warnings).
- Weight gain varies depending on the SSRI.
- Sexual side effects may include delayed or loss of orgasm and low sexual drive.
- Paroxetine may cause heart-related birth defects if taken during the first 3 months of pregnancy. The most common heart abnormalities are ventricular septal defects, which are holes in the muscular wall that separate the main pumping chambers of the heart. Pregnant women who are being treated for major depression should not stop taking antidepressants without first talking to their doctors. [For more information on antidepressant treatment guidelines during pregnancy, see "Treating Depression During and After Pregnancy" in Treatment section.]
- Citalopram can cause serious heart rhythm problems if taken in doses higher than 40mg/day (or 20 mg/day for people age 60 years and older). People with certain underlying heart conditions, including heart failure and recent heart attack, should not take citalopram in any dose. Let your doctor know if you experience irregular heartbeat, dizziness, or shortness of breath while taking this drug.
- SSRIs can worsen manic symptoms in people with bipolar disorder.
Drug Interactions
SSRIs can interact with other antidepressants such as tricyclics and, in particular, monoamine oxidase inhibitors (MAOIs). Due to a potentially fatal condition called serotonin syndrome, SSRIs should never be taken in combination with an MAOI or within 2 weeks after discontinuing MAOI treatment. (For more on serotonin syndrome, see the MAOI section below.) Other serious interactions can occur with meperidine (Demerol, generic) and illegal substances (such as LSD, cocaine, or ecstasy). SSRIs also interact with the antibiotic linezolid (Zyvox), opioid painkillers such as tramadol (Ultram, generic), mood stabilizers containing lithium, and cough medicines containing dextromethorphan. People who take SSRIs may drink alcohol in moderation, although the combination may compound any drowsiness experienced with SSRIs, and some SSRIs increase the effects of alcohol.
Withdrawal Symptoms
Cognitive problems, sleep disturbances, increase in depressive symptoms, and electric shock-like symptoms can occur with sudden discontinuation of SSRIs. The symptoms are more likely to occur with antidepressants with shorter half-lives as compared with fluoxetine, which has a long half-life. The dose of the antidepressant should be slowly reduced before stopping.
Other Neurotransmitter Inhibitors
These antidepressants target other neurotransmitters, such as norepinephrine or dopamine, alone or in addition to serotonin.
Dual Action Inhibitors
Dual action inhibitors act directly on serotonin and another neurotransmitter.
Venlafaxine (Effexor, generic), desvenlafaxine (Pristiq), duloxetine (Cymbalta, generic), mirtazapine (Remeron), and levomilnacipran (Fetzima) are serotonin norepinephrine reuptake inhibitors (SNRIs). They target serotonin and the neurotransmitter norepinephrine and are approved for treatment of major depression in adults.
These drugs share many of the side effects of SSRIs, including dry mouth, nausea, and drowsiness. Additional side effects include:
- Venlafaxine (Effexor, generic) and desvenlafaxine (Pristiq) can increase blood pressure and heart rate and should be used with caution in people with high blood pressure or heart disease. They can also cause uterine and vaginal bleeding unrelated to menstruation. Venlafaxine and desvenlafaxine should not be taken during the last trimester of pregnancy as they can cause complications in newborn infants. Some people report severe withdrawal symptoms, including dizziness and nausea.
- Duloxetine (Cymbalta, generic) can worsen narrow-angle glaucoma and liver or kidney problems. Because duloxetine can cause liver damage, people who drink large quantities of alcoholic beverages should not take it. Signs of liver damage include itching, dark urine, yellowing of skin and eyes (jaundice), and fatigue. People should immediately contact their doctor if they experience these symptoms.
- Mirtazapine (Remeron) can cause impulsivity, panic attacks, and restlessness.
Multiple Neurotransmitter Inhibitors (Bupropion)
Bupropion (Wellbutrin, generic) affects the reuptake of serotonin, norepinephrine, and dopamine -- a third important neurotransmitter. In addition to depression, bupropion is also approved for treating seasonal affective disorder (SAD) and, under the trade name Zyban, for smoking cessation. Bupropion causes less sexual dysfunction than SSRIs. About 25% of people experience initial weight loss. Side effects include restlessness, agitation, sleeplessness, headache, and stomach problems. Bupropion has a risk for seizures, which increases with higher doses. High doses may also cause dangerous heart arrhythmias.
Tricyclic Antidepressants
Before the introduction of SSRIs, tricyclics were the standard treatment for depression.
Tricyclics are sometimes grouped into two categories:
- Tertiary amines include amitriptyline (Elavil, Endep, generic) and imipramine (Tofranil, generic).
- Secondary amines include desipramine (Norpramin, generic) and nortriptyline (Pamelor, Aventyl, generic). Secondary amines may have fewer side effects, including drowsiness, than tertiary amines, but they are as toxic in high amounts.
Less commonly used tricyclics include doxepin (Sinequan), amoxapine (Asendin), maprotiline (Ludiomill), protriptyline (Vivactil), and trimipramine (Surmontil). These are all available as generics.
Tricyclics are as effective for treating depression but they have many side effects. They may offer benefits for many people with dysthymia, who generally do not respond to SSRIs. They may also be prescribed in lower dosages to be taken at night to help with insomnia.
Side Effects of Tricyclics
Side effects are common with these medications. In an analysis of studies, more tricyclic users discontinued their drugs due to side effects than did SSRI or MAOI users. Side effects most often reported include:
- Dry mouth
- Constipation
- Blurred vision
- Sexual dysfunction
- Weight gain
- Difficulty urinating
- Drowsiness
Tricyclics can have serious, although rare, side effects:
- They tend to cause disturbances in heart rhythm, which can pose a danger for some people with certain heart diseases. Care should be taken when these medications are prescribed to older people and to those at risk of overdose. In particular, desipramine (Norpramin, generic) has been associated with dangerous heart rhythm abnormalities in people who have a family history of these problems.
- Tricyclics, particularly imipramine, may increase the risk for a lung disease called idiopathic pulmonary fibrosis (IPF), which can cause lung inflammation and scarring. Initial symptoms are breathlessness and dry cough.
- Tricyclics can cause dizziness associated with orthostatic hypotension, a sudden drop in blood pressure when sitting up or suddenly standing.
- Tricyclics can be fatal with an overdose.
Serotonin Modulators
Serotonin modulators work to increase the effect of serotonin in the brain. These drugs include trazodone (Desyrel), serzone (Nefazodone), and vilazodone (Viibryd). They may be used to treat major depression and premenstrual syndrome.
Side Effects of Tricyclics
Side effects may occur with these medications. Side effects most often reported include:
- Dry mouth
- Dizziness
- Constipation
- Blurred vision
- Difficulty urinating
- Drowsiness
Serotonin modulators may interact with other antidepressant medicines:
- Serotonin modulators may not be used along with MAO inhibitors.
- They may also interact adversely with SSRIs and Lithium.
Monoamine Oxidase Inhibitors (MAOIs)
Monoamine oxidase inhibitors (MAOIs) block monoamine oxidase, an enzyme which has negative effects on many of the neurotransmitters that are important for well-being. MAOIs include phenelzine (Nardil, generic), isocarboxazid (Marplan, generic), and tranylcypromine (Parnate, generic).
Newer MAOIs, such as selegiline (Eldepryl, Movergan, generic), target only one form of the MAOI enzyme. They may cause fewer side effects than older MAOIs. A skin patch form of selegiline (Emsam) is also available for treatment of major depressive disorder in adults.
Because these drugs can have very severe side effects, they are usually prescribed only for severe depression or when other types of antidepressants do not help (treatment-resistant depression). MAOIs may also be effective for the following conditions:
- Eating disorders
- Post-traumatic stress disorder
- Borderline personality
Side Effects
MAOIs commonly cause the following side effects:
- Orthostatic hypotension (a sudden drop in blood pressure upon standing).
- Drowsiness or insomnia.
- Dizziness.
- Sexual dysfunction.
- The most serious side effect is severe hypertension (high blood pressure), which can be brought on by eating certain foods having high tyramine content. Such foods include aged cheeses, most red wines, sauerkraut, vermouth, chicken livers, dried meats and fish, canned figs, fava beans, and concentrated yeast products.
- MAOIs can cause birth defects and should not be taken by pregnant women.
Serotonin Syndrome
Serotonin syndrome is a potentially fatal condition that can occur from interactions of MAOIs with other antidepressants, including SSRIs. Symptoms include confusion, agitation, sweating and shivering, and muscle spasms. There should be at least a 2-week break between taking MAOIs and other antidepressants. MAOIs can have serious interactions with other drugs as well, including some common over-the-counter cough medications. In such cases, severe high blood pressure or dangerous reactions can occur. It is important that people discuss with their doctors any other medications they are taking.
Atypical Antipsychotics
If people fail to respond to antidepressants, doctors may try adding on a different type of drug. (This combination strategy is called "augmentation" or "adjunctive treatment".) Atypical antipsychotics are drugs that are usually prescribed for schizophrenia or bipolar disorder, but may in certain circumstances also play a role in the treatment of severe depression.
Two atypical antipsychotics, aripiprazole (Abilify) and quetiapine (Seroquel, generic), are currently approved in combination with antidepressant therapy for treatment of adults with major depressive disorder. A third approved medication called Symbyax (generic), combines in one pill the atypical antipsychotic olanzapine (Zyprexa, generic) with the SSRI fluoxetine (Prozac, generic).
Atypical antipsychotics can have a number of serious side effects. They include:
- Sedation
- Weight gain, metabolic problems, and increased risk for type 2 diabetes
- Unhealthy cholesterol levels and heart problems
- Extrapyramidal symptoms such as tardive dyskinesia, which are severe and uncontrollable movement disorders
If you are prescribed an atypical antipsychotic, your doctor should carefully monitor your weight, blood sugar (glucose) levels, cholesterol levels, and any signs that may indicate the emergence of extrapyramidal symptoms.
Investigational Drugs
Ketamine
Ketamine, an anesthetic drug, may be helpful for people with severe treatment-resistant or bipolar depression, although it is not approved by the FDA for this use. In preliminary studies, a single intravenous dose of ketamine helped people quickly recover from depression within several hours, and some people sustained benefits for up to a week. (Standard antidepressant drugs usually take about 8 weeks to have an effect.) Evidence of benefit after one or more weeks is less clear. Ketamine blocks the NMDA brain protein receptor, which is involved in glutamate regulation. Glutamate is a brain chemical that is thought to be involved in depression. Ketamine may have serious side effects including hallucinations, irrational behavior, and increased blood pressure. Ketamine can also induce dependence and is sometimes used as a drug of abuse.
- Psychotherapy
Among the various psychotherapeutic "talk therapies," cognitive behavioral therapy appears to be the most effective approach. If psychotherapy is used alone without medications, benefits should be evident within 8 weeks and symptoms should be fully resolved by 12 weeks. If these conditions are not met, then the person should strongly consider antidepressant drugs.
Cognitive Behavioral Therapy
For many people, cognitive behavioral therapy (CBT) works as well as antidepressants in treating severe depression. Like all psychotherapies, much of the success depends on the skill of the therapist. Many studies suggest that combining cognitive therapy with antidepressants offer the greatest benefits. Studies also indicate that the benefits of cognitive therapy persist after treatment has ended.
CBT focuses on identification of distorted perceptions that people may have of the world and themselves, on changing these perceptions, and on discovering new patterns of actions and behavior. These perceptions, known as schemas, are negative assumptions developed in childhood that can precipitate and prolong depression. CBT works on the principle that these schemas can be recognized and altered, thereby changing the response and eliminating the depression.
- First, the person learns to recognize depressive reactions and thoughts as they occur, usually by keeping a journal of feelings about, and reactions to, daily events.
- The person is often given "homework" that tests old negative assumptions against reality and demands different responses.
- Then, the person and therapist examine and challenge these entrenched and automatic reactions and thoughts.
- As people begin to understand that the beliefs and assumptions that cause depression are incorrect, they can begin substituting new, positive ways of coping.
Over time, such exercises help build confidence and eventually alter behavior. People may take group or individual cognitive therapy. CBT is a time-limited treatment, typically lasting 12 to 14 weeks.
Psychodynamic Therapy and Interpersonal Therapy (IPT)
Psychodynamic therapy is a form of talk therapy that focuses on uncovering internal conflicts and unresolved issues that stem from childhood. Psychodynamic therapy evolved from Freudian psychoanalysis and includes the theories of Freud's followers (Adler, Jung, Erickson).
Interpersonal therapy is a form of psychodynamic therapy that acknowledges the childhood roots of depression, but focuses on symptoms and current issues that may be causing problems. IPT is not as specific as cognitive behavioral therapy, and all work is done during the sessions. The therapist seeks to redirect the person's attention, which has been distorted by depression, toward the daily details of social and family interaction.
The goals of this treatment method are improved communication skills and increased self-esteem within a short period of time (3 to 4 months of weekly appointments). Among the forms of depression best served by IPT are those caused by distorted or delayed mourning, unexpressed conflicts with people in close relationships, major life changes, and isolation.
- Other Treatments
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) is commonly called shock treatment. It has received bad press, in part for its potential memory-depleting effect. Since its introduction in the 1930s, ECT has been significantly refined, and is now considered an effective and safe treatment for severe depression in the appropriate situation. It is especially effective for people who have not been helped by medication and those with severe depression who experience delusions and hallucinations. Maintenance ECT may also help prevent relapse.
Candidates for ECT
ECT may be helpful for the following people with severe and complex depression with the following features:
- People who cannot take antidepressant drugs or who have not been helped by drug therapy
- People with major depression with psychotic or catatonic features
- Suicidal people
- Older people who are psychotic and depressed
- People with severe postpartum depression
- Young people who fit the adult criteria for ECT
The Procedure
In general, hospitalization is not necessary. ECT involves the following steps:
- People receive a muscle relaxant and short-acting anesthetic.
- A small amount of electric current is sent to the brain, causing a generalized seizure that lasts for about 40 seconds.
- Most people receive 6 treatments, spaced every 2 to 5 days. Others receive up to 15 treatments, followed by 6 to 12 additional treatments spaced every other week or longer for another 2 to 4 months.
Side Effects
Side effects of ECT may include temporary confusion, memory lapses, headache, nausea, muscle soreness, and heart disturbances. Concerns about permanent memory loss appear to be unfounded. More recent studies showed that cognitive side effects may be minimized by changes in electrode placement and in the electrical signal characteristics.
The ECT procedure affects heart rate and blood pressure. Doctors should perform a medical evaluation of people before they receive ECT. People, (especially those who are older), who have high blood pressure, atrial fibrillation, asthma, or other heart or lung problems may be at increased risk for heart-related side effects.
Transcranial Direct Current Stimulation (tDCS)
Researchers are studying a potential alternative to ECT called Transcranial Direct Current Stimulation (tDCS). It is a non-invasive approach that uses weak direct electric currents to stimulate the front of the brain through electrodes placed on the scalp. Unlike ECT, treatment is given for 20 to 30 minutes at a time, and people remain conscious throughout the procedure. In preliminary studies, tDCS produced good results in people with severe, treatment-resistant depression and did not cause the memory problems associated with ECT. TDCS is an investigational procedure, only available in clinical trials. It is not yet FDA-approved.
Transcranial Magnetic Stimulation and Deep Brain Stimulation
Repetitive transcranial magnetic stimulation (rTMS) uses high frequency magnetic pulses that target affected areas of the brain. It is generally regarded as a second line treatment after ECT. Researchers are continuing to refine rTMS techniques to attempt to improve treatment outcomes.
An implantable deep brain stimulation device (Reclaim), similar to a pacemaker and devices used for treating movement disorders like Parkinson disease, has been approved for treatment of severe obsessive-compulsive disorder. It is currently in clinical trials for treatment-resistant depression.
The device uses 4 electrodes that are surgically implanted into the brain and connected to a small generator that is implanted near the abdomen or collar bone. The generator delivers precisely controlled electrical pulses to target specific areas of the brain. Other types of deep brain stimulation for severe depression are also being studied in clinical trials.
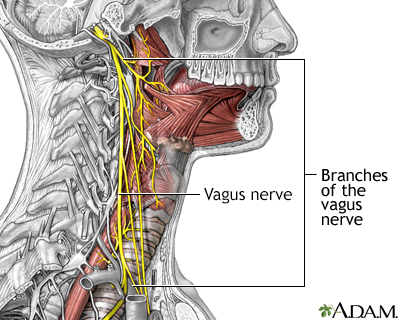
Vagus Nerve Stimulation
Vagus nerve stimulation (VNS) is a procedure that is effective for certain patients with epilepsy, and is now showing some success in people with treatment-resistant depression.
VNS involves implanting a battery-powered device under the skin in the upper left of the chest. The neurologist programs the device to deliver mild electrical stimulation to the vagus nerve. The two vagus nerves are the longest nerves in the body. They run along each side of the neck, then down the esophagus to the gastrointestinal tract. The vagus nerve travels to areas of the brain that control functions such as sleep and mood.
Studies report good response rates in appropriate candidates with treatment-resistant depression. VNS is approved by the FDA for long-term treatment of chronic depression in adults who have not responded to typical treatments for their major depressive episode. People who use VNS may continue to show improvement in both their depression symptoms and quality of life.
Vagal stimulation can cause shortness of breath, hoarseness, sore throat, coughing, ear and throat pain, or nausea and vomiting. These side effects can be reduced or eliminated by reducing the intensity of stimulation. Long-term studies on people with epilepsy have reported no serious adverse side effects, although the treatment may cause lung function deterioration in some people with existing lung disease.
The vagus nerves branch off the brain on either side of the head and travel down the neck, along the esophagus to the intestinal tract. They are the longest nerves in the body, and affect swallowing and speech. The vagus nerves also connect to parts of the brain involved in seizures. In many seizures disorders, electrical stimulation of the vagus nerves may help relieve symptoms.
Phototherapy (Light Therapy)
Phototherapy, also called light therapy, may be recommended as treatment for seasonal affective disorder (SAD), particularly for people who do not wish to use antidepressants.
The procedure is noninvasive and simple. It is best performed immediately after waking in the morning. People sit a few feet away from a box-like device that emits very bright fluorescent light (10,000 lux) for about 30 minutes every day.
Some people report mood improvement as early as 2 days after treatment. In others, depression may not lift for 3 to 4 weeks. If no improvement is experienced after that, depressive symptoms will be unlikely to respond to phototherapy. Phototherapy may work best when combined with cognitive behavioral therapy.
Side effects include headache, eye strain, and irritability, although these symptoms tend to disappear within a week. People taking light-sensitive drugs (such as those used for psoriasis), certain antibiotics, or antipsychotic drugs should not use light therapy. People should be examined by an ophthalmologist before undergoing this treatment.
Music Therapy
Studies have shown that adding music therapy to regular treatment for depression improves the treatment result. Music therapy has short-term beneficial effects in people with depression of all ages and can also decrease anxiety levels in depressed people.
Acupuncture
There is some evidence that acupuncture may reduce the severity of depression. It is not clear however whether acupuncture provides any additional relief when given together with medication or psychotherapy as compared to those therapies alone. More studies are needed.
- Lifestyle Changes
Exercise and Other Healthy Behaviors
Exercise
Both aerobic exercise and resistance training can help provide some improvement in mood symptoms for people with depression. Aerobic workouts can raise chemicals in the brain, such as endorphins, adrenaline, serotonin, and dopamine that produce the so-called runner's high. Yoga practice, which involves rhythmic stretching movements and breathing, may help improve and stabilize mood. Meditation may also be helpful.
Sleep Hygiene
People with depression who suffer from insomnia (either as a result of the condition or medications) may be helped by learning sleep hygiene techniques. Research also suggests that cognitive behavioral therapy for insomnia may help depression treatment.
Nutrition and Diet
A healthy diet low in saturated fats and rich in whole grains, fresh fruits, and vegetables is important for anyone. People should be sure to maintain a regular healthy diet, particularly if they have experienced weight gain from medications. They should also try to decrease their use of alcohol and tobacco.
Social Support
A strong network of social support is important for both prevention and recovery from depression. Support from family and friends should be healthy and positive. The more that family members become educated about depression, the better they can understand this illness and provide support.
Herbal Remedies and Dietary Supplements
Generally, manufacturers of herbal remedies and dietary supplements do not need FDA approval to sell their products. Just like a drug, herbs and supplements can affect the body's chemistry, and therefore have the potential to produce side effects that may be harmful. There have been a number of reported cases of serious and even lethal side effects from herbal products. Always check with your doctor before using any herbal remedies or dietary supplements.
St. John's wort
St. John's wort (Hypericum perforatum) is probably the most studied herbal remedy. Although its efficacy has not been consistently proven in thorough clinical studies, there is some evidence it may help certain people with mild-to-moderate depression. It does not help people with severe depression. St. John's wort and other herbal remedies should not be used in place of conventional anti-depressive therapy.
The herb St. John's wort is believed to be helpful in relieving mild-to-moderate depression, but should only be taken under a doctor's supervision. Manufacturers of herbal supplements do not need FDA approval to sell their products.
The following guidelines are recommended:
- People with depression should not use St. John's wort without consulting a doctor. Children and pregnant or nursing women should not take this substance.
- St. John's wort should not be combined with other antidepressant medication. This herb may also interact with other types of medications and increase or decrease their potency. St. John's wort can increase the risk of bleeding when used with blood-thinning drugs. It can also reduce the strength of certain drugs including those used for cancer and HIV treatments.
Side effects are uncommon but may include nausea, dry mouth, allergic reactions, and fatigue. This herb may increase sensitivity to light (photosensitivity).
S-adenosyl methionine (SAM-e)
S-adenosyl methionine, better known as SAM-e, is a molecule found in the human body and is involved in the processing of the neurotransmitters dopamine and serotonin. Studies have shown that levels of SAMe are lower in people with severe major depressive disorder. Some studies have indicated that SAM-e dietary supplements may be helpful for people with depression, but the evidence is still limited and more data are needed.
Fish Oil
Some studies have suggested omega-3 fatty acids may be helpful for depression. Omega-3 fatty acids are found in fish oil, canola oil, soybeans, flaxseed, and certain nuts and seeds. The omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are also available in combination dietary supplement form. Some research has suggested that the Mediterranean diet, which is high in omega-3 rich foods as well as vegetables and fruit and low in saturated fats from meat, may help reduce the risk of developing depression.
Omega-3 fatty acids, found in oily fish and flaxseed and canola oils, may be beneficial to people with depression.
Vitamins
Certain B vitamins may be associated with some protection against depression.
- Vitamin B-3 (niacin) is important in the production of tryptophan, the precursor of serotonin, and is produced from processing vitamin B3 (niacin). Dietary sources of niacin include oily fish (such as salmon or mackerel), pork, chicken, dried peas and beans, whole grains, seeds, and dried fortified cereals.
- Low levels of folate, a B vitamin, may be associated with depression. Researchers are studying whether folate supplements may help enhance the effectiveness of SSRIs and other antidepressants. The American Psychiatric Association notes that folate supplements carry little risk (and can help prevent birth defects), and it may be reasonable for people to take folate along with drug therapy.
- Resources
- National Institute of Mental Health -- www.nimh.nih.gov
- Depression and Bipolar Support Alliance -- www.dbsalliance.org
- National Alliance on Mental Illness -- www.nami.org
- Mental Health America -- www.mhanational.org
- American Academy of Child and Adolescent Psychiatry -- www.aacap.org
- Postpartum Support International -- www.postpartum.net
References
Aalbers S, Fusar-Poli L, Freeman RE, et al. Music therapy for depression. Cochrane Database Syst Rev. 2017;11:CD004517. PMID: 29144545 pubmed.ncbi.nlm.nih.gov/29144545/.
Baek JH, Nirenberg AA, Fava M. Pharmacological approaches to treatment-resistant depression. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 44.
Bostic JQ, Prince JB, Buxton DC. Child and adolescent psychiatric disorders. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 69.
Chokka PR, Hankey JR. Assessment and management of sexual dysfunction in the context of depression. Ther Adv Psychopharmacol. 2018;8(1):13-23. PMID: 29344340 pubmed.ncbi.nlm.nih.gov/29344340/.
Fava M, Østergaard SD, Cassano P. Mood disorders: depressive disorders (major depressive disorder). In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 29.
Fava M, Papakostas GI. Antidepressants. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Psychopharmacology and Neurotherapeutics. Philadelphia, PA: Elsevier; 2016:chap 3.
Fava M, Papakostas GI. Antidepressants. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 43.
Kok RM, Reynolds CF 3rd. Management of depression in older adults: a review. JAMA. 2017;317(20):2114-2122. PMID: 28535241 pubmed.ncbi.nlm.nih.gov/28535241/.
Malhi GS, Mann JJ. Depression. Lancet. 2018;392(10161):2299-2312. PMID: 30396512 pubmed.ncbi.nlm.nih.gov/30396512/.
Nonacs RM, Wang B, Viguera AC, Cohen LS. Psychiatric illness during pregnancy and the post-partum period. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 31.
Park LT, Zarate CA Jr. Depression in the Primary Care Setting. N Engl J Med. 2019;380(6):559-568. PMID: 30726688 pubmed.ncbi.nlm.nih.gov/30726688/.
Perez DL, Murray ED, Price BH. Depression and psychosis in neurological practice. In: Daroff RB, Jankovic J, Mazziotta JC, Pomeroy SL, eds. Bradley's Neurology in Clinical Practice. 7th ed. Philadelphia, PA: Elsevier; 2016:chap 10.
Siu AL, US Preventive Services Task Force (USPSTF), Bibbins-Domingo K, et al. Screening for depression in adults: US Preventive Services Task Force recommendation statement. JAMA. 2016;315(4):380-387. PMID: 26813211 pubmed.ncbi.nlm.nih.gov/26813211/.
Smith CA, Armour M, Lee MS, Wang LQ, Hay PJ. Acupuncture for depression. Cochrane Database Syst Rev. 2018;3:CD004046. PMID: 29502347 pubmed.ncbi.nlm.nih.gov/29502347/.
Vaccarino V, Bremner JD. Psychiatric and behavioral aspects of cardiovascular disease. In: Zipes DP, Libby P, Bonow RO, Mann DL, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 11th ed. Philadelphia, PA: Elsevier; 2019:chap 96.
Walter HJ, DeMaso DR. Mood disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21th ed. Philadelphia, PA: Elsevier; 2020:chap 39.
Welch CA. Electroconvulsive therapy. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 45.
Yonkers KA. Management of depression and psychoses in pregnancy and in the puerperium. In: Resnik R, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 67.